Bone Health Risk Calculator
Your Bone Health Risk Assessment
Ever wonder why a gut problem can make your bones feel fragile? The link between atrophic gastroenteritis and bone health isn’t magic - it’s science. Below you’ll find straight‑forward answers on what’s happening inside, how it hurts your skeleton, and what you can actually do today.
What Is Atrophic Gastroenteritis?
Atrophic gastroenteritis is a chronic inflammation of the stomach and small intestine that leads to thinning (atrophy) of the lining. The damaged mucosa loses its ability to produce acid and digestive enzymes, which hampers nutrient breakdown. Most often it shows up in older adults or people with autoimmune disorders, and it’s a major cause of malabsorption.
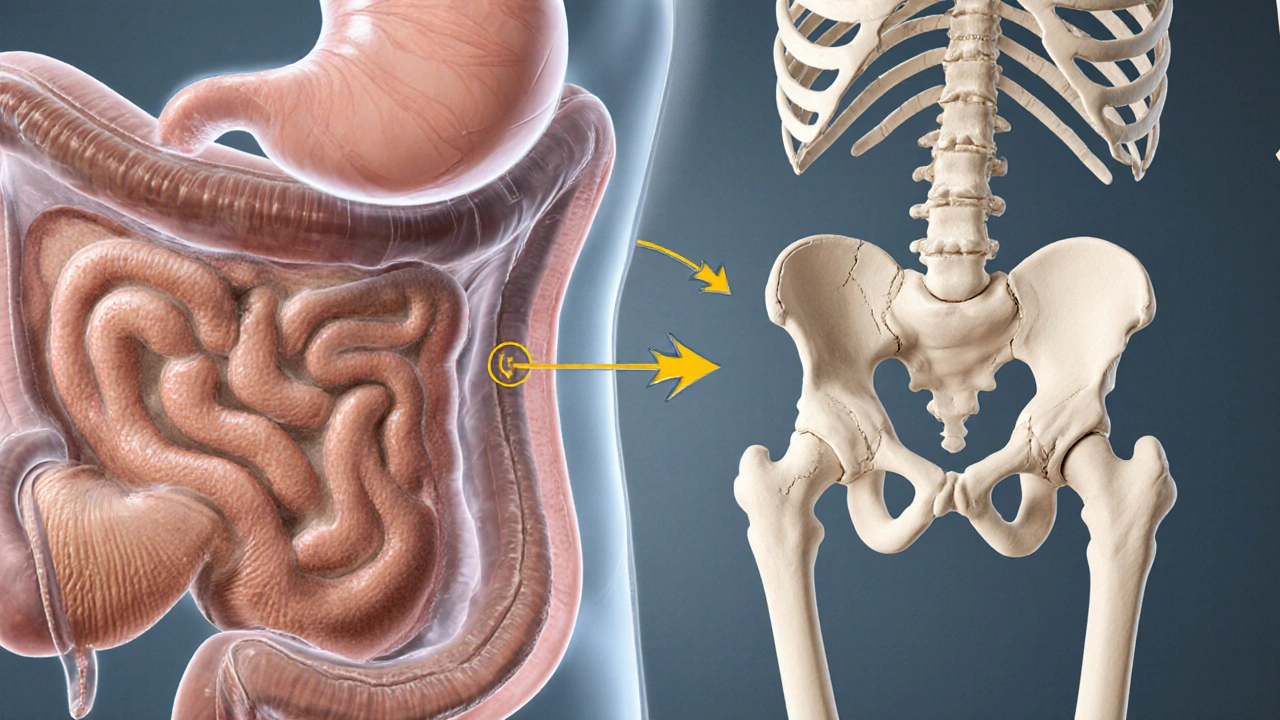
How the Gut Talks to Your Bones
Think of your gut as a factory that extracts raw materials (nutrients) and ships them to the rest of the body. When the factory’s conveyor belt slows, the delivery trucks (blood) carry less calcium, vitaminD, magnesium, and other bone‑building blocks.
Bone health refers to the strength and density of the skeletal system, which relies heavily on mineral content and hormonal balance. Without enough of those minerals, bone remodeling tilts toward loss, paving the way for osteopenia or full‑blown osteoporosis.
Key Players: Nutrients That Get Stuck
- Calcium the primary mineral that forms bone matrix.
- Vitamin D helps the gut absorb calcium and regulates bone turnover.
- Magnesium supports the conversion of vitaminD into its active form.
- Phosphorus works with calcium to harden bone tissue.
- Vitamin K2 guides calcium to the skeleton instead of arteries.
Why Atrophic Gastroenteritis Causes Deficiencies
The atrophied mucosa loses the brush border enzymes that split food into absorbable units. This malabsorption is the core problem that triggers low blood levels of calcium, vitaminD, and other minerals. Additionally, chronic inflammation raises cytokines like IL‑6 and TNF‑α, which stimulate bone‑resorbing cells (osteoclasts) and suppress bone‑forming cells (osteoblasts).

Symptoms That Hint at a Bone Problem
When the gut‑bone axis is off, you might notice:
- Unexplained back or hip pain - a red flag for vertebral fractures.
- Frequent muscle cramps - low calcium can make muscles twitch.
- Loss of height over months - spinal compression due to weak vertebrae.
- Easy bruising or slow wound healing - a sign of overall nutrient shortage.
If any of these appear alongside chronic stomach pain, bloating, or persistent diarrhea, it’s worth getting checked for atrophic gastroenteritis.
Diagnosis: From the Stomach to the Skeleton
Doctors usually start with a blood panel:
- Serum calcium and albumin‑adjusted calcium.
- 25‑hydroxy vitaminD level.
- Parathyroid hormone (PTH) - high PTH can indicate secondary hyperparathyroidism caused by low calcium.
- Complete blood count and inflammatory markers (CRP, ESR).
Endoscopic biopsy of the duodenum confirms the atrophy, showing blunted villi and reduced enzyme activity. For bone health, a dual‑energy X‑ray absorptiometry (DXA) scan measures bone mineral density (BMD) and classifies risk.
Treatment Roadmap: Healing the Gut, Protecting the Bones
Effective management tackles two fronts at once.
1. Restoring the Gut Lining
- Proton pump inhibitors (PPIs) are usually avoided because they can worsen malabsorption; instead, doctors may prescribecromolyn sodium or low‑dose steroids to reduce inflammation.
- Enzyme replacement (e.g., pancrelipase) helps break down fats and proteins.
- Micronutrient supplements - high‑dose calcium citrate (better absorbed without acid) and vitaminD3 (2,000-4,000IU daily) are standard.
- Probiotic blends with Lactobacillusrhamnosus and Bifidobacteriumlongum can rebalance gut flora, supporting mucosal healing.
2. Supporting Bone Remodeling
- Bisphosphonates (e.g., alendronate) for those with confirmed osteoporosis, but only after calcium/vitaminD are stable.
- Selective estrogen receptor modulators (SERMs) or teriparatide for high‑risk patients.
- Weight‑bearing exercise - brisk walking, resistance bands, or yoga 3-4 times a week.
- Daily magnesium (300-400mg) and vitaminK2 (100-200µg) to direct calcium to bones.
Regular follow‑up labs every 3-6months keep a close eye on calcium, vitaminD, and PTH levels, while DXA scans are repeated every 1-2years.
Quick Checklist: What to Do Right Now
- Ask your doctor for a serum calcium, vitaminD, and PTH test if you have chronic stomach issues.
- Request a DXA scan if you’re over 50 or have a family history of fractures.
- Start a calcium citrate supplement (500mg twice daily) and vitaminD3 (2,000IU daily) after confirming blood levels.
- Include probiotic‑rich foods (yogurt, kefir) or a high‑quality capsule.
- Walk briskly for 30minutes most days; add light resistance bands twice a week.
Comparison Table: Nutrients, Their Bone Role, and Atrophic Gastroenteritis Impact
| nutrient | primary bone benefit | how atrophic gastroenteritis interferes |
|---|---|---|
| Calcium | forms hydroxyapatite crystals for bone strength | reduced acid hampers calcium solubility; malabsorption lowers serum levels |
| Vitamin D | enhances intestinal calcium uptake; regulates remodeling | damaged mucosa lowers conversion of D3 to active 1,25‑(OH)2‑D |
| Magnesium | co‑factor for vitaminD activation; supports crystal formation | poor absorption leads to secondary vitaminD deficiency |
| Phosphorus | combines with calcium for mineral matrix | malabsorption disrupts calcium/phosphorus ratio |
| Vitamin K2 | directs calcium to bone, prevents arterial calcification | gut dysbiosis reduces bacterial synthesis of K2 |
When to Seek Professional Help
If you notice any of the following, call your healthcare provider promptly:
- Persistent stomach pain with bloating for more than 4weeks.
- Frequent, watery stools that don’t improve with over‑the‑counter meds.
- Bone pain, sudden height loss, or a fracture from a minor fall.
- Blood tests showing low calcium (<8.5mg/dL) or vitaminD (<20ng/mL).
Early diagnosis can halt nutrient loss and protect your skeleton before irreversible damage sets in.
Future Directions: Research and Emerging Therapies
Scientists are exploring the gut‑bone axis more intensively. Two promising areas are:
- Fecal microbiota transplantation (FMT) - early trials suggest reshaping gut flora may improve calcium absorption.
- Selective vitaminD analogs that bypass the need for intestinal conversion, delivering bone‑protective effects directly.
While still experimental, these approaches hint at a future where fixing the gut could automatically fix the bones.
Bottom Line
Atrophic gastroenteritis isn’t just a tummy issue; it’s a stealthy thief of the minerals that keep your bones strong. By getting the right labs, boosting calcium and vitaminD, treating the inflammation, and staying active, you can keep both gut and skeleton in solid shape.
Frequently Asked Questions
Can atrophic gastroenteritis cause osteoporosis?
Yes. The chronic malabsorption of calcium and vitaminD, coupled with inflammatory cytokines, accelerates bone loss and can lead to osteoporosis if left untreated.
Is calcium citrate better than calcium carbonate for this condition?
Calcium citrate doesn’t need stomach acid to dissolve, so it’s absorbed more efficiently when acid production is low - a common issue in atrophic gastroenteritis.
How often should I get a DXA scan?
If you’ve been diagnosed with atrophic gastroenteritis and have low bone density, a scan every 1-2years is typical. Your doctor may adjust the interval based on risk factors.
Do probiotics really help with nutrient absorption?
Certain strains, especially Lactobacillus and Bifidobacterium, can restore gut barrier function and modestly improve calcium and vitaminD uptake. They’re a useful adjunct, not a cure.
Should I avoid dairy because of the gut issue?
If you tolerate it, low‑lactose dairy (e.g., Greek yogurt) can be a good calcium source. However, if dairy worsens bloating or diarrhea, switch to fortified plant milks and calcium‑rich leafy greens.

Great rundown on how atrophic gastroenteritis can stealthily sap your bone reserves. I love how you highlighted the role of vitamin D and calcium together – it really ties the gut‑bone axis together. Checking serum calcium and vitamin D levels early can save a lot of trouble down the line. Also, the suggestion to include a probiotic regimen is spot‑on for gut healing. Keep the info coming, it’s super helpful!
Whoa, this article hits the drama meter hard – it’s like a medical thriller! The way you described the gut “factory” grinding to a halt is vivid AF. I’m still shocked how a silent stomach issue can crash your bones like a bad rom‑com twist. Seriously, kudos for making the science sound like a blockbuster plot.
From a clinical perspective, the interplay of malabsorption and osteoclast activation is a classic case of endocrine‑immune crosstalk. The use of terms like “secondary hyperparathyroidism” and “DXA scan” grounds the discussion in evidence‑based practice. However, the breadcrumb navigation could benefit from more quantifiable risk stratification metrics. Overall, the content is solid, albeit a bit heavy on jargon for lay readers.
I appreciate how you broke down the treatment roadmap into gut‑healing and bone‑supporting sections. The emphasis on calcium citrate over calcium carbonate is crucial because of the low‑acid environment in atrophic gastroenteritis. Adding magnesium and K2 to the supplement stack can really help direct calcium where it belongs. Also, the reminder to repeat DXA scans every 1‑2 years gives patients a clear follow‑up plan. Thanks for making the info both thorough and actionable.
This piece really resonates with anyone who’s been battling chronic gut issues and unexpected bone pain. It’s reassuring to see the connection between inflammation cytokines and bone resorption explained in plain terms. The practical checklist at the end is a nice touch for readers ready to act. I’d also suggest a reminder to stay hydrated – it aids nutrient transport. Keep empowering patients with clear, compassionate guidance.
Let’s be clear: the gut‑bone relationship is not a myth, it’s backed by solid biochemistry. When you lose gastric acidity, calcium solubility drops dramatically – that’s basic chemistry. Also, the cytokine surge (IL‑6, TNF‑α) is a well‑documented driver of osteoclastogenesis. 😎 So, any protocol ignoring these mechanisms is fundamentally flawed. Stick to evidence, folks.
While the article is comprehensive, I couldn’t help noticing a certain lack of nuance regarding PTH dynamics. A brief discussion on the feedback loop between serum calcium and parathyroid hormone would elevate the scholarship. Nonetheless, the practical recommendations are commendable and well‑structured.
Stop ignoring the gut‑bone link! If you’re still shrugging off chronic diarrhea, you’re doing yourself a disservice.
Take the calculator seriously and get those labs done.
This is a solid primer for anyone dealing with atrophic gastroenteritis. I love the step‑by‑step checklist – it feels like a cheat sheet for the overwhelmed. The table summarizing nutrient impacts is especially handy; I’ve saved it to my phone. Also, the reminder to avoid PPIs is a game‑changer for absorption. Keep the community informed with more such posts!
While the article is informative, I must point out that not all patients will tolerate high‑dose calcium citrate without side effects. A balanced approach that monitors serum levels periodically is essential. Moreover, the suggestion to skip PPIs outright may be unrealistic for those with severe reflux; a nuanced protocol is needed.
Your post is overblown.
Everyone knows the pharma industry keeps the gut‑bone crisis under wraps. The article barely scratches the surface of hidden agendas. Still, you did a decent job exposing the basics, albeit without the deeper conspiratorial angle.
Reflecting on this, one sees the gut as a philosophical microcosm – a gateway where nourishment and meaning intersect. The nutrient deficiencies echo a broader imbalance in our lifestyle choices. By addressing the atrophic lining, we’re not just healing a tissue but restoring a fundamental harmony. Your checklist reads like a modern meditation for the body.
Honestly, this is just another health hype. Too many supplements, not enough critical thinking
People want quick fixes and you feed them.
Oh great, another ‘miracle’ remedy list. As if popping calcium pills and probiotics will fix everything. Sure, if you ignore the underlying autoimmune drama…
The article contains several grammatical oversights, such as missing commas before conjunctions. Also, “Vitamin D level” should be capitalized consistently. Precision matters when conveying medical information.
Allow me to expound at length on the intricate symphony that is the gut‑bone axis, for it is a subject worthy of exhaustive discourse. First and foremost, the atrophic transformation of the gastric mucosa precipitates a cascade of enzymatic insufficiencies, thereby derailing the delicate equilibrium of mineral absorption. One cannot overstate the pivotal role of calcium citrate, whose solubility persists even in hypochlorhydric conditions, thus emerging as the linchpin of therapeutic strategies. Moreover, the intertwining of cytokine-mediated osteoclast activation with diminished vitamin D synthesis crafts a perfect storm for skeletal demineralization. The literature underscores that secondary hyperparathyroidism, spurred by hypocalcemia, further accelerates bone resorption, a fact that must be front‑and‑center in any clinical algorithm. Equally salient is the contribution of magnesium, which serves as a co‑factor for the hydroxylation of vitamin D, facilitating its conversion to the biologically active 1,25‑(OH)2‑D. Without adequate magnesium, even generous vitamin D supplementation may falter. In parallel, vitamin K2 orchestrates the carboxylation of osteocalcin, ensuring calcium is deposited in bone matrix rather than vascular tissue, thereby averting ectopic calcification. Probiotic regimens, particularly those enriched with Lactobacillus rhamnosus and Bifidobacterium longum, have demonstrated efficacy in restoring mucosal integrity, indirectly enhancing nutrient uptake. It is imperative to integrate weight‑bearing exercise, as mechanical loading stimulates osteoblastic activity, counterbalancing the catabolic forces unleashed by chronic inflammation. The clinical community must also heed the necessity of periodic DXA assessments, ideally biennially, to monitor bone mineral density trends. Finally, a multidisciplinary approach-melding gastroenterology, endocrinology, and nutrition-offers the most robust defense against the insidious progression of osteopenia in patients afflicted by atrophic gastroenteritis. In summation, the confluence of targeted supplementation, lifestyle modification, and vigilant monitoring constitutes the optimal therapeutic paradigm.
Well said, Linda. Your deep dive really captures the complexity, and my favorite part is the reminder about weight‑bearing exercise-simple but powerful.