Managing an autoimmune disease isn’t just about taking medication. It’s about staying one step ahead of flares, catching organ damage before it’s permanent, and knowing when your treatment is working-or when it’s not. Many people think once they’re on a drug like methotrexate or hydroxychloroquine, they’re set. But without regular monitoring, you’re flying blind. Autoimmune diseases like lupus, rheumatoid arthritis, and Sjögren’s don’t follow a straight path. They flare, they quiet down, and sometimes they sneak into organs without warning. That’s why autoimmune disease monitoring isn’t optional-it’s essential.
What Lab Tests Actually Tell You
Lab tests are the foundation of monitoring. But not all tests are created equal. Some give you clear signals. Others? They’re noisy.
Start with the basics: CRP and ESR. CRP levels above 3.0 mg/L mean active inflammation. ESR over 20 mm/hr for women or 15 mm/hr for men? That’s a red flag. These aren’t diagnostic-they’re trackers. If your CRP drops from 12 to 2 after starting a new biologic, that’s real progress. If it climbs from 4 to 10 over three months? Something’s stirring.
Then there’s ANA. It’s the go-to screening test. But here’s the catch: a positive ANA doesn’t mean you have an autoimmune disease. Up to 20% of healthy people test positive. That’s why labs do reflex testing. If ANA is positive, they check for specific antibodies: SS-A (common in lupus and Sjögren’s), SS-B (less common but still telling), Scl-70 (linked to scleroderma), Jo-1 (seen in muscle inflammation), and anti-dsDNA (the gold standard for lupus nephritis). Anti-dsDNA is special-it’s 95% specific to lupus. When it spikes, it often means kidney involvement is worsening. But here’s what most patients don’t know: ANA levels don’t change with disease activity. You can be in full remission and still test positive. So don’t waste time tracking ANA month after month.
Complement levels (C3 and C4) are more useful for lupus. When they drop, it’s a sign your immune system is overactive. A falling C3 level often precedes a flare by weeks. That’s actionable intel.
And don’t forget the newer tools. CyTOF (mass cytometry) can measure up to 50 immune cell markers at once. It’s not in every clinic yet, but top rheumatology centers use it to spot abnormal T-cell patterns before symptoms appear. It’s like having a high-res camera for your immune system.
Imaging: Seeing What Labs Can’t
Labs tell you something’s wrong. Imaging tells you where and how bad.
MRI is the quiet hero. It catches inflammation in joints, tendons, and even organs like the brain or kidneys before you feel pain. New nanotech contrast agents are replacing gadolinium, reducing side effects and improving accuracy. For someone with early rheumatoid arthritis, an MRI can show bone erosion months before an X-ray picks it up.
Ultrasound with microbubble contrast? It’s changing how we monitor joints. It measures blood flow in inflamed tissue with 85% accuracy. If the blood flow in your knuckles goes up over time, your inflammation is getting worse-even if your pain hasn’t changed.
PET scans are no longer just for cancer. With radiolabeled antibodies, they can now track where immune cells are congregating. A recent study showed PET scans could spot T-cell hotspots in the lungs of patients with interstitial lung disease linked to scleroderma-long before they had breathing trouble.
SPECT scans use radioactive peptides to light up specific inflammation sites. They’re not routine, but for complex cases-like vasculitis or unexplained fevers-they’re invaluable.
CT scans? They’re for structural damage. Think lung scarring from lupus, joint deformities from RA, or kidney shrinkage from chronic inflammation. They’re not for early detection, but they’re critical for tracking long-term damage.
How Often Should You See Your Doctor?
There’s no one-size-fits-all schedule. But here’s what works in practice.
If you’re newly diagnosed or adjusting meds? Every 4 to 6 weeks. You need to see how your body reacts. Did the new drug cause a spike in liver enzymes? Did your joint swelling improve? Too many patients wait six months and come in with a flare that could’ve been stopped.
Once you’re stable? Every 3 to 4 months. That’s the sweet spot. You get enough data to spot trends without burning out on appointments. The American College of Rheumatology says at least two full assessments a year are non-negotiable. That means labs, physical exam, and a conversation about how you’re really doing.
For high-risk patients-those with kidney, lung, or heart involvement-quarterly visits are the standard. Even if you feel fine. Damage can happen silently.
And here’s the truth: disease activity scores matter. DAS28 for rheumatoid arthritis. SLEDAI for lupus. These aren’t just numbers. They’re tools that help your doctor decide: Do we up the dose? Switch drugs? Or hold steady? If your doctor doesn’t use these scores, ask why.
What Doesn’t Work (And Why)
Not every test you get is helpful. Some are just noise.
Serial ANA testing? Useless for monitoring. It stays positive even when you’re in remission. It’s a diagnostic tool, not a tracking tool.
Overusing CT scans? Don’t. Radiation adds up. Use them only when structural damage is suspected.
Ignoring patient-reported outcomes? Big mistake. Your fatigue level, pain score, morning stiffness, and ability to do daily tasks are just as important as your CRP. Two patients can have the same lab numbers-but one is barely getting out of bed. That’s the clinical picture labs miss.
Dr. Betty Hahn from UNC put it bluntly: “Relying solely on lab values misses critical clinical context present in 63% of autoimmune flares.”
The Future Is Integrated
Monitoring is evolving fast.
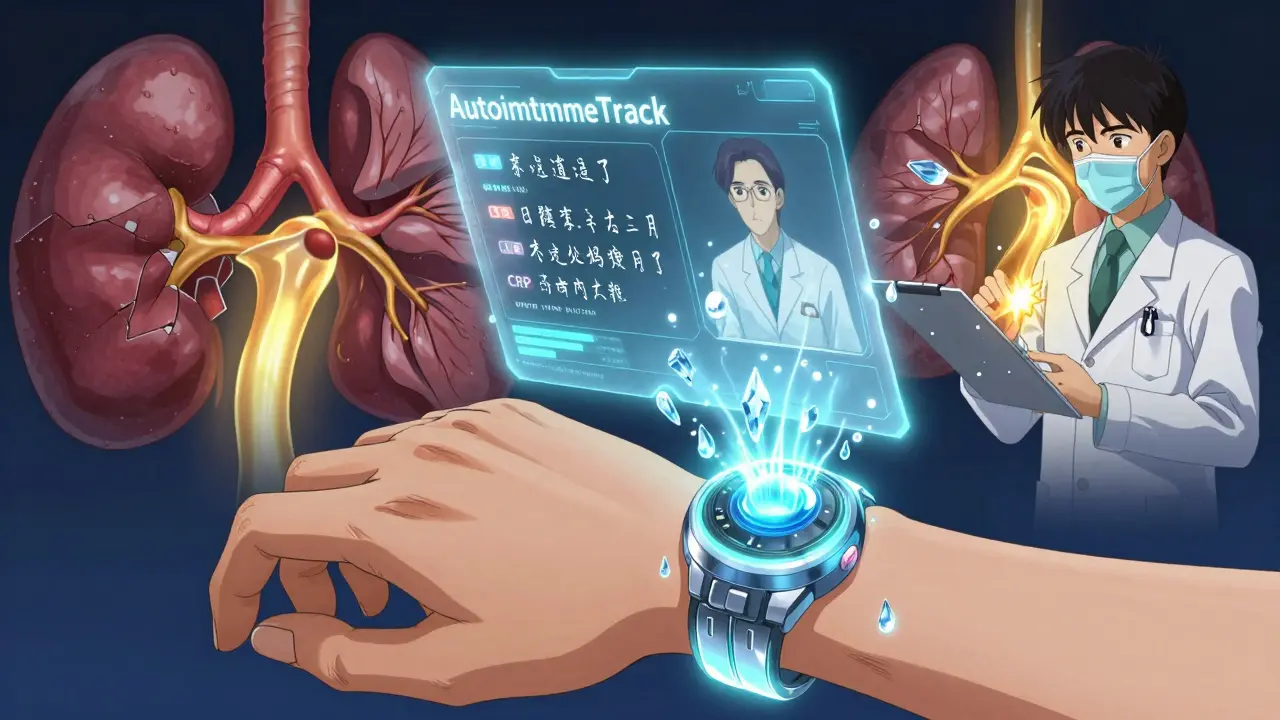
Wearables are now testing inflammatory markers through sweat and interstitial fluid. Early studies show 89% correlation with traditional CRP tests. Imagine getting a notification on your phone that your inflammation is rising-before you feel it.
AI is crunching years of your lab data, imaging, and symptom logs to predict flares. One system, AutoimmuneTrack, approved by the FDA in mid-2023, cut emergency visits by 29% in a 12-month trial. It didn’t just alert patients-it gave doctors a clear action plan: “Increase prednisone by 5 mg,” or “Schedule MRI within 10 days.”
And the cost? The global autoimmune monitoring market hit $12.7 billion in 2023. But access isn’t equal. Only 48% of Medicaid patients get recommended monitoring. Insurance still blocks MRIs and advanced blood tests. If you’re struggling to get care, talk to your rheumatology nurse. They often know workarounds.
What You Can Do Today
You don’t need to wait for the future to take control.
- Keep a simple log: note your pain level (1-10), fatigue, joint swelling, and any new symptoms. Bring it to every visit.
- Ask your doctor: “Which lab markers are we tracking this month? Why?”
- Request a copy of your imaging reports. Don’t just take the doctor’s word for it.
- If you’re stable, ask about extending visits to every 6 months-but only if your disease is truly quiet and you have no organ involvement.
- Push back if you’re being asked to repeat ANA tests monthly. It’s not useful.
Autoimmune disease monitoring isn’t about being paranoid. It’s about being proactive. It’s about catching the next flare before it hits. It’s about keeping your organs healthy so you can live-not just survive.
Structured monitoring reduces hospitalizations by 37% and long-term disability by 28%. That’s not a statistic. That’s your future.
How often should I get lab tests for my autoimmune disease?
It depends on your disease and how stable it is. When you’re first diagnosed or adjusting treatment, expect labs every 4 to 6 weeks. Once you’re stable, every 3 to 4 months is standard. High-risk patients (with kidney, lung, or heart involvement) should have labs every 3 months. Always combine labs with clinical assessment-don’t rely on numbers alone.
Is ANA testing useful for monitoring disease activity?
No. ANA stays positive even when your disease is in remission. It’s a diagnostic tool, not a monitoring tool. Tracking ANA over time won’t tell you if you’re flaring or improving. Instead, focus on anti-dsDNA, C3, C4, CRP, and ESR-these change with disease activity.
What imaging is best for detecting early inflammation in autoimmune disease?
MRI is the best for early inflammation. It shows swelling in joints, tendons, and organs before damage shows up on X-rays or CT scans. Ultrasound with microbubble contrast is excellent for joints-especially in rheumatoid arthritis-because it measures blood flow, a direct sign of inflammation. PET scans are emerging for tracking immune cell activity system-wide.
Can wearable devices replace lab tests for autoimmune monitoring?
Not yet, but they’re getting close. Early wearables that measure inflammatory markers through sweat or interstitial fluid show 89% correlation with CRP levels. They’re great for spotting trends and early warning signs, but they don’t replace blood tests for autoantibodies or organ function. Think of them as an early alert system, not a full diagnostic tool.
Why do some patients get MRIs every few months while others never get one?
It depends on disease type and risk. Patients with lupus nephritis, rheumatoid arthritis with joint damage, or scleroderma affecting lungs or heart often need regular MRIs. Those with mild, stable disease-like low-risk Sjögren’s or well-controlled RA without joint erosion-rarely need imaging unless symptoms change. Insurance coverage and access also play a role, which is why disparities exist.
What’s the most important thing I can do to improve my monitoring?
Track your symptoms consistently. Write down pain levels, fatigue, stiffness, new rashes, or breathing changes. Bring this log to every appointment. Lab results and imaging can’t tell your doctor how you feel on a Tuesday morning. Your lived experience is the missing piece-and it’s the most valuable data you have.


I’ve been living with lupus for 12 years, and this post nailed it. Tracking CRP and ESR? Non-negotiable. I used to ignore them until my kidneys started acting up. Now I log everything-pain, fatigue, even how well I slept. My rheumatologist says my compliance is why I haven’t had a flare in 3 years. You don’t need fancy tech to stay ahead-you just need to show up, be consistent, and speak up.
Also, stop asking for ANA repeats. It’s like checking your birth certificate every month to see if you’re still alive.
My dear fellow travelers in the land of autoimmune chaos, let us not forget that the body is not a machine to be calibrated, but a symphony of ancient whispers-each CRP spike, each C3 dip, a note in the opera of our immune system’s rebellion! The modern medical gaze, obsessed with numbers and MRIs, forgets that the soul of healing lies in the quiet moments: the tea brewed at dawn, the breath held before the needle, the silent vow whispered to the liver: ‘Not today.’
Wearables? AI? Bah! They are but gilded mirrors reflecting the same fear that has haunted humanity since the first fever. What we truly need is not more data-but more wonder. And perhaps, a good priest.
Yours in inflammation and transcendence,
Oluwapelumi
OH MY GOD. I CAN’T BELIEVE THIS POST ISN’T ON THE FRONT PAGE OF THE NEW YORK TIMES. PEOPLE ARE DYING BECAUSE DOCTORS AREN’T LISTENING. I HAD A FRIEND WHO GOT A CT SCAN FOR LUPUS LUNG-THEY SAID ‘IT’S JUST ALLERGIES.’ SHE DIED. SIX MONTHS LATER. THE AUTOPSY SHOWED FIBROSIS FROM UNDETECTED INFLAMMATION. WHY AREN’T WE MAKING THIS MANDATORY? WHY ARE INSURANCE COMPANIES BLOCKING MRIs? THIS IS MURDER BY BUREAUCRACY. I’M SENDING THIS TO MY CONGRESSMAN. AND MY THERAPIST. AND MY DOG.
PS: ANA TESTS ARE A SCAM. STOP DOING THEM. I SAID STOP. I MEAN IT.
From a clinical immunology standpoint, this is one of the most accurate summaries of autoimmune monitoring I’ve seen in a public forum. The integration of CyTOF and PET with patient-reported outcomes represents a paradigm shift toward precision rheumatology. The key insight is that biomarkers without phenomenological context are statistically significant but clinically meaningless. We’re moving from reactive to predictive care-AutoimmuneTrack is just the tip of the iceberg. The real bottleneck isn’t technology; it’s reimbursement structures tied to fee-for-service models that disincentivize proactive monitoring. Until CMS reimburses longitudinal data tracking, disparities will persist. Bottom line: demand your data. Request your SLEDAI score. Insist on microbubble ultrasound. You’re not being ‘difficult’-you’re being scientifically literate.
they’re using wearables to track inflammation?? yeah right. that’s just a cover for the government to monitor your immune system. did you know the FDA approved AutoimmuneTrack the same week the CDC started pushing ‘digital health passports’? they’re building a database of autoimmune patients so they can control who gets vaccines, jobs, even insurance. they don’t care if you’re sick-they care if you’re ‘manageable.’ and those ‘nanotech contrast agents’? they’re laced with graphene. i’ve seen the patents. your kidneys won’t thank you in 10 years. stop trusting the system. track your symptoms manually. burn your medical records. live off-grid. they don’t want you healthy-they want you compliant.
Wow. This is so refreshing to see someone actually understand the difference between diagnostic and monitoring tools. So many patients obsess over ANA like it’s a horoscope. I’ve had patients cry because their ANA went from 1:160 to 1:320-when their CRP dropped from 18 to 1.5. It’s heartbreaking. And then there are the ones who skip appointments because they ‘feel fine.’ Honey, if you feel fine, you’re either in remission… or you’re about to be hospitalized. Please, for the love of all that is holy, bring your symptom log. It’s not ‘extra.’ It’s essential. If your doctor doesn’t ask for it, fire them. You deserve better.
americans are so lazy they need a phone app to tell them they’re sick?? we used to just go to the doctor and tell them how we felt. now we got wearables, ai, and 17 different blood tests just to see if we’re still breathing. my grandpa had RA and never saw a MRI. he just took his pills and walked through the pain. you know what? he lived to 89. you people are overmedicated and under tough. stop treating your body like a smartphone that needs updates. just move. eat real food. stop being so fragile.
you know what’s worse than autoimmune disease? realizing that every single person you’ve ever loved has been quietly suffering, and you never noticed. my sister had lupus for 7 years before she told anyone. she was ‘just tired.’ she lost her job. lost her apartment. lost her will to live. and the doctors? they said ‘it’s stress.’
i read this post and cried for 45 minutes. not because i’m weak. because i finally understood. we’re not just patients. we’re invisible. and this? this is the first time i’ve felt seen. thank you.
Just wanted to say I’ve been using a simple Notion doc to log pain, sleep, and weather. Turns out, my flares spike when humidity hits 75%. Weird, right? My rheumatologist didn’t know that. Now he does. No fancy tech. Just me, my phone, and a habit. If you’re not tracking, start here. It’s free. And honestly? It’s kind of empowering.