Chronic Alcohol Use Disorder (AUD) isn't just about drinking too much. It's a medical condition where your brain and body become wired to need alcohol-even when it's destroying your health, relationships, and future. You might still be able to hold a job or show up for family events, but inside, your body is screaming for more. And the longer it goes untreated, the more damage piles up-often silently, until it's too late.
How Chronic AUD Changes Your Body
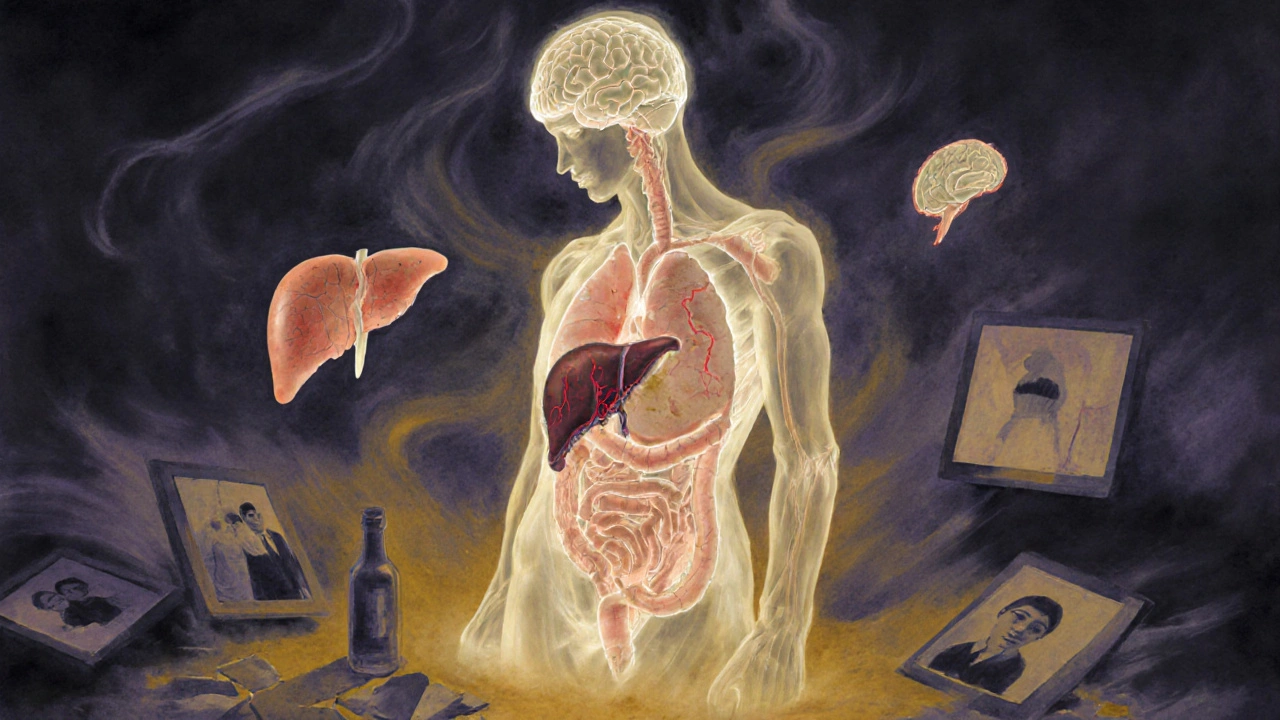
Your body doesn’t handle alcohol the way it handles water or coffee. Every drink hits your liver first, and over time, that organ gets overwhelmed. Around 90% of heavy drinkers develop fatty liver disease, where fat builds up in liver cells. At this stage, you might feel fine. No pain. No symptoms. But the damage is happening.
If drinking continues, it moves to alcoholic hepatitis-your liver becomes inflamed, cells die, and you start feeling nauseous, weak, or jaundiced. Then comes cirrhosis: scar tissue replaces healthy liver tissue. Once cirrhosis sets in, your liver can’t filter toxins, make proteins, or store energy properly. Some damage can reverse if you stop drinking, but not all. The liver has limits.
But it’s not just your liver. Alcohol messes with your brain. Long-term use shrinks brain tissue, especially in areas that control decision-making and impulse control. You might notice memory lapses, trouble focusing, or mood swings that don’t go away. Heavy drinkers are up to 2.7 times more likely to get pneumonia because alcohol weakens your immune system. Your heart isn’t safe either. Drinking heavily raises your risk of high blood pressure, irregular heartbeat (atrial fibrillation), and stroke by 34%. One drink a day increases breast cancer risk by 12%. Five drinks a day? Your mouth, throat, and esophagus cancer risk jumps fivefold.
What Happens When You Stop
If you’ve been drinking daily for months or years, quitting cold turkey can be dangerous. Your nervous system has adapted to alcohol’s presence. When it’s gone, your brain goes into overdrive. Symptoms can start within hours: shaky hands, sweating, nausea, anxiety. Within 24-48 hours, you might experience hallucinations or seizures. In severe cases, delirium tremens (DTs) can occur-fever, confusion, rapid heartbeat, and even death if untreated.
This is why medical detox is critical for people with moderate to severe AUD. It’s not about comfort-it’s about survival. Hospitals and specialized clinics use medications like benzodiazepines to calm the nervous system and prevent seizures. They also replace nutrients your body lost-especially thiamine (vitamin B1). Without it, you risk Wernicke’s encephalopathy, a brain disorder that causes confusion, loss of coordination, and eye movement problems. Left untreated, it can lead to permanent memory loss.
Medications That Help You Stay Sober
Medication isn’t a magic pill, but it’s one of the most underused tools in AUD treatment. Three FDA-approved drugs are proven to help:
- Naltrexone (ReVia, Vivitrol): Blocks the pleasurable effects of alcohol. If you drink while on it, you don’t get the usual rush. This reduces cravings over time.
- Acamprosate (Campral): Helps restore brain chemistry after stopping. It’s most effective after detox, especially for people who feel anxious, restless, or emotionally unstable.
- Disulfiram (Antabuse): Makes you sick if you drink. It causes nausea, vomiting, and flushing. It’s not for everyone, but for some, the fear of getting sick is enough to keep them sober.
Studies show that combining medication with counseling increases abstinence rates by 24% compared to counseling alone. Yet, only about 1 in 5 people with AUD ever get these medications. Many still think recovery means just “willpower.” It doesn’t. AUD is a brain disorder-and like diabetes or hypertension, it often needs medicine to manage.

Therapy: Rewiring Your Relationship With Alcohol
Medication helps with the body. Therapy helps with the mind. Cognitive Behavioral Therapy (CBT) is one of the most effective approaches. It teaches you to spot triggers-stress, boredom, certain people or places-and replace drinking with healthier responses. In studies, CBT reduces heavy drinking days by 60% over six months.
Motivational Enhancement Therapy (MET) works differently. It’s not about pushing you to quit. It’s about helping you find your own reasons. Many people with AUD feel stuck. They know they should stop, but they’re scared of life without alcohol. MET helps you explore that fear and build motivation from within.
Group therapy matters too. Alcoholics Anonymous (AA) has helped millions since 1935. Their 12-step program isn’t for everyone, but their peer support system works. One 2014 survey found 27% of members stayed abstinent after one year. Critics say the data isn’t perfect, but the real-world impact is undeniable: people show up, they talk, they stay accountable. Newer options like SMART Recovery focus on science-backed tools instead of spirituality, giving people more choices.
Emerging Treatments and What’s Next
Treatment isn’t stuck in the 1980s. New tools are emerging. Transcranial Magnetic Stimulation (TMS)-a non-invasive brain stimulation technique-showed 50% abstinence rates in a 2022 study. It targets areas of the brain involved in cravings. The FDA has also approved digital therapeutics like the reSET app, which delivers CBT through a smartphone. In trials, users were twice as likely to stay sober compared to those who didn’t use it.
These aren’t replacements for traditional care. They’re additions. For people who can’t access therapists, live in rural areas, or feel ashamed to walk into a clinic, apps and remote care make help possible.

The Hidden Costs: Beyond Health
AUD doesn’t just hurt your body. It destroys your life. People lose jobs. Relationships fall apart. Savings vanish. In the U.S., excessive alcohol use cost $249 billion in 2010-mostly from lost productivity, healthcare, and criminal justice expenses. Alcohol was involved in 29% of all traffic deaths in 2016. It’s linked to domestic violence, homelessness, and suicide.
And yet, only 19.2% of the 14.5 million Americans with AUD got treatment in 2019. That’s not a failure of will. It’s a failure of access. Stigma keeps people silent. Insurance doesn’t always cover therapy or meds. Many clinics are overcrowded or hard to reach.
Recovery isn’t linear. Relapse is common. But it doesn’t mean failure. It means the treatment plan needs adjusting. The goal isn’t perfection-it’s progress. One day sober. One week. One year.
You’re Not Alone
Chronic AUD is not a moral failing. It’s a medical condition with biological roots. Your brain changed because of alcohol-not because you’re weak. And the good news? It can change back-with the right support.
If you’re reading this and thinking, ‘I might have a problem,’ you’re already on the path to recovery. The first step isn’t quitting forever. It’s talking to someone-a doctor, a counselor, a trusted friend. You don’t have to do it alone. Treatment works. People recover. And it’s never too late to start.
Can you recover from liver damage caused by chronic alcohol use?
Yes, in many cases. Early-stage liver damage like fatty liver can reverse completely if you stop drinking. Alcoholic hepatitis can improve significantly with abstinence. Even some cirrhosis cases show stabilization or partial healing over time. But once scar tissue becomes widespread, it’s permanent. The key is stopping before the damage is irreversible. The sooner you quit, the better your chances.
Is AUD the same as alcoholism?
Yes, but the term "alcoholism" is outdated. Since 2013, the medical community uses "Alcohol Use Disorder" (AUD) to describe the full spectrum-from mild to severe. What people used to call "alcoholism" is now classified as severe AUD. The change was made to reduce stigma and reflect that it’s a medical condition, not a character flaw.
What’s the difference between binge drinking and AUD?
Binge drinking means consuming a lot of alcohol in a short time-5+ drinks for men, 4+ for women-in about 2 hours. It’s a behavior. AUD is a diagnosis based on multiple symptoms: loss of control, cravings, tolerance, withdrawal, and continued use despite harm. Someone can binge drink without having AUD. But repeated binge drinking increases the risk of developing it.
Can medications for AUD be used long-term?
Yes. Unlike some addiction treatments, AUD medications like naltrexone and acamprosate are designed for long-term use-sometimes for years. Think of them like blood pressure pills: they help manage a chronic condition. Stopping them too soon increases relapse risk. Your doctor will help you decide how long to stay on them based on your progress and needs.
Why do some people relapse after treatment?
Relapse is common because AUD changes the brain’s reward system. Triggers-stress, emotions, places, people-can spark cravings even after months or years of sobriety. It doesn’t mean treatment failed. It means the recovery plan needs strengthening. Many people benefit from ongoing therapy, support groups, or medication adjustments after a relapse. Recovery is a process, not a one-time event.
Are there alternatives to Alcoholics Anonymous?
Yes. AA is one option, but not the only one. SMART Recovery uses science-based tools like cognitive behavioral techniques. Refuge Recovery blends mindfulness with Buddhist principles. Women for Sobriety focuses on gender-specific needs. There are also online communities and apps like Sober Grid and Inebriate. The key is finding a group that feels right for you-not just what’s traditional.
Can AUD be treated without going to rehab?
For mild to moderate AUD, yes. Many people successfully recover with outpatient therapy, medication, and support groups without residential rehab. Detox may still be needed if you’re physically dependent, but that can often be done safely in a clinic without staying overnight. Rehab is typically recommended for severe AUD, co-occurring mental health issues, or if home support is lacking.
How long does it take to feel normal after quitting alcohol?
It varies. Withdrawal symptoms peak in 2-3 days and fade within a week. But brain chemistry takes months to stabilize. Sleep, mood, and energy levels often improve over 3-6 months. Some people report feeling emotionally clearer after a year. Patience matters. Healing isn’t overnight-but it does happen.
Does AUD affect mental health?
Absolutely. AUD and mental health conditions like depression, anxiety, and PTSD often go hand in hand. Alcohol may seem to help at first, but it worsens symptoms over time. Many people with AUD are also diagnosed with depression. Treating both together-called dual diagnosis treatment-leads to much better outcomes than treating one alone.
Is it safe to quit alcohol cold turkey?
Only if you’ve been drinking lightly or occasionally. If you’ve been drinking daily for months or years, quitting suddenly can cause seizures, delirium tremens, or even death. Medical supervision during detox is essential. Never attempt to quit heavy drinking alone without consulting a doctor first.

So let me get this straight - we’ve got a medical condition that rewires your brain, destroys your liver, and costs the economy $250 billion a year… but the solution is still ‘just quit’? 🤡
Meanwhile, my cat gets more consistent healthcare than someone with AUD. We treat high blood pressure with pills. Why the hell is AUD still treated like a moral failing? 😤
It’s not merely a biochemical imbalance - it’s a metaphysical collapse of personal responsibility. The modern addiction paradigm, while clinically convenient, obfuscates the deeper existential failure: the surrender of the will to the chemical seduction of dopamine. 🧠🍷
And yet, we offer naltrexone like it’s a spiritual sacrament. How quaint. We’ve replaced confession with pharmacology.
I lost my brother to this. He was 32. They told him ‘just stop.’ He tried. He cried. He failed. Then he died alone in a motel.
Stop talking about ‘options.’ Start fixing the system.
Wait - so you’re telling me that if I drink 5 drinks a day, I’m 5x more likely to get throat cancer… but if I drink 4.9, I’m fine? 🤔
Also, who decided ‘heavy drinking’ is 5 drinks? That’s like saying ‘obese’ is 10 lbs over your BMI. Arbitrary. Also, I heard the FDA approves apps now? Next they’ll prescribe TikTok for PTSD.
So… you’re saying AA works because ‘people show up’? That’s it? No peer-reviewed data? No control groups? Just… vibes? 🙄
And you call that science? Meanwhile, I’ve been sober for 11 years using cognitive restructuring, no god, no steps, just logic. But no one wants to hear that. Too real.
Y’all are overcomplicating this. Stop drinking. That’s it. No meds. No apps. No therapy. Just say no. I’ve seen 3 people quit cold turkey and now they run marathons. Your brain isn’t broken - you’re just weak. 💪
Also, why is everyone so obsessed with ‘recovery’? Just be normal. 😌
This is one of the clearest, most compassionate breakdowns of AUD I’ve ever read. Seriously - thank you.
For anyone reading this and thinking ‘I can’t do this’ - you already did the hardest part: you’re here. You’re learning. That’s courage.
Medication isn’t cheating. Therapy isn’t weakness. Asking for help isn’t failure - it’s the most powerful thing you’ll ever do. You’ve got this. One day at a time.
Who funded this article? Big Pharma? The rehab industrial complex? They’re pushing meds to keep you dependent - not free.
And why is ‘TMS’ suddenly a miracle? Last year it was ketamine. Next year it’ll be AI therapists.
Real recovery is discipline. Not gadgets. Not pills. Not apps. Just willpower. The system wants you addicted to treatment - not sober.
Wait, so naltrexone blocks pleasure… but what if I just like the taste of whiskey? 🤔
Also, I read somewhere that alcohol is good for your heart? Or was that wine? Or was that a study funded by a vineyard? I’m confused now.
And why is AA still around? Isn’t that like using a rotary phone in 2024? 😅
Hey, I’ve been sober 8 months after 12 years of heavy drinking. Didn’t use meds. Used therapy, yoga, and a really good podcast. But I get it - it’s not one-size-fits-all.
What helped me most? Knowing I wasn’t broken. Just wounded. And wounds heal - but they need time, care, and people who don’t judge.
If you’re reading this and scared - I was too. But you’re not alone. Reach out. Even just to a stranger on Reddit. I’ll reply.
Let’s be clear: AUD is a chronic neurobiological disorder, akin to Type 2 Diabetes or Hypertension - with a behavioral component that requires both pharmacological and psychosocial intervention.
The failure of our healthcare system lies not in the science, but in the stigma, fragmented access, and insurance barriers that prevent 80% of patients from receiving evidence-based care.
Medication-assisted treatment reduces mortality by up to 50%. Yet, only 19% receive it. This isn’t a moral crisis - it’s a policy failure. And it’s killing people.
Advocacy, funding, and destigmatization aren’t optional. They’re urgent.
It’s all a construct. The ‘disease model’ was invented by psychiatrists in the 1950s to legitimize their profession. Alcohol has been consumed since antiquity - yet only now is it a ‘disorder’?
Meanwhile, the real epidemic is the erosion of personal sovereignty. We’ve outsourced our will to pills, apps, and therapists. We’ve become patients, not people.
True freedom is choosing sobriety without a prescription. But who wants to hear that?