Duloxetine Liver Monitoring Calculator
Liver Monitoring Calculator
Important Information
According to the article, 78% of significant liver enzyme spikes happen between 8-12 weeks (56-84 days) after starting duloxetine. For high-risk patients, additional testing at 4 months may be recommended.
What to Watch For
Signs of liver injury include yellow skin or eyes (jaundice), dark urine, nausea, fatigue, itching, and abdominal pain. If you experience these symptoms, contact your doctor immediately.
When you start taking duloxetine for depression, anxiety, or chronic pain, your main focus is usually how quickly you’ll feel better-not whether it might hurt your liver. But here’s the reality: duloxetine carries a real, though rare, risk of liver damage that many patients and even some doctors don’t fully understand. If you’re on this medication-or thinking about it-you need to know the signs, the timeline, and what steps to take to stay safe.
What Is Duloxetine, and Why Does It Affect the Liver?
Duloxetine, sold under the brand name Cymbalta, is a serotonin-norepinephrine reuptake inhibitor (SNRI). It’s approved for major depression, generalized anxiety disorder, diabetic nerve pain, fibromyalgia, and chronic back or muscle pain. It works by boosting two key brain chemicals that affect mood and pain signals. But here’s the catch: your liver breaks down duloxetine using enzymes called CYP1A2 and CYP2D6. Sometimes, this process creates small, harmful byproducts that can damage liver cells.
This isn’t just theoretical. Clinical trials show that about 1-2% of people taking duloxetine at the standard 60 mg daily dose develop elevated liver enzymes. In about 0.6% of cases, those enzymes rise more than three times the normal upper limit-enough to signal real stress on the liver. The damage usually shows up as a hepatocellular pattern: ALT and AST levels spike, sometimes dramatically. That’s the same pattern seen in alcohol-related liver injury or viral hepatitis.
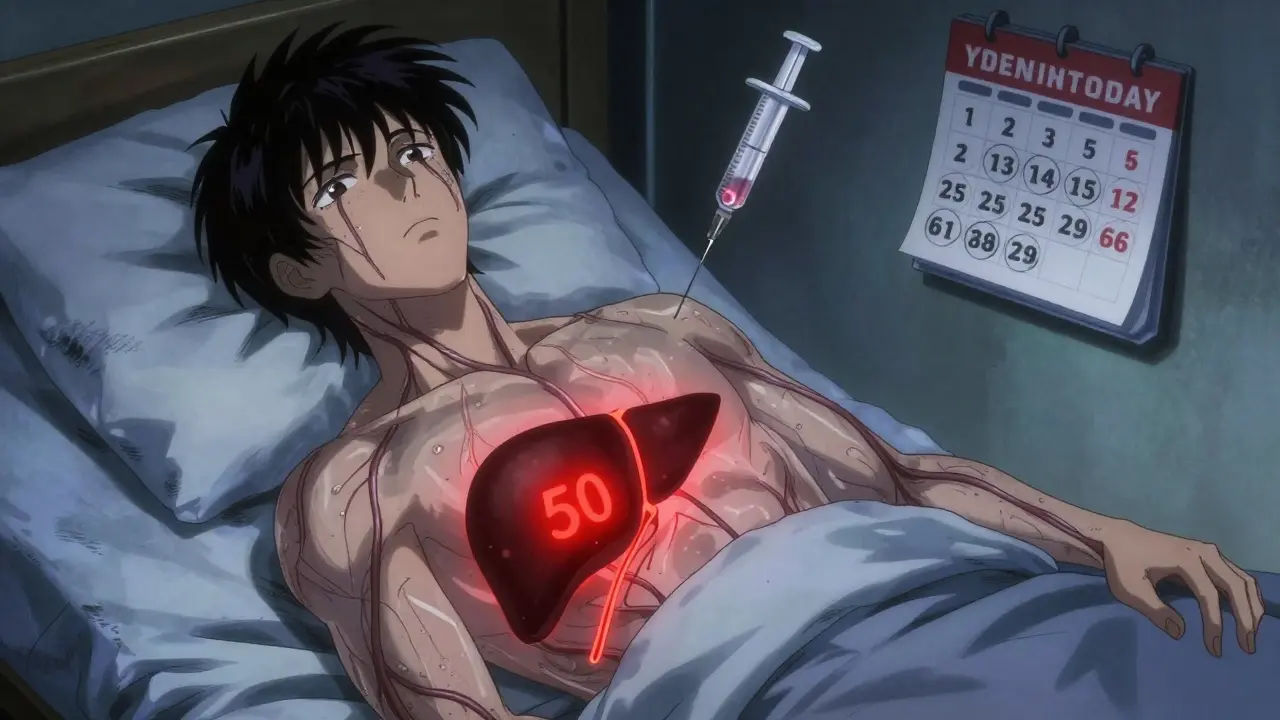
When Does Liver Damage Happen?
One of the most dangerous things about duloxetine-related liver injury is how predictable the timing is. Most cases show up between 35 and 62 days after starting the drug. The median time? Around 50 days. That’s not a random fluke-it’s a pattern seen across dozens of case reports and clinical studies.
Here’s why this matters: if you get your liver tests done only at your first appointment and then never again, you’re flying blind during the highest-risk window. Many patients feel fine during this time. No nausea, no fatigue, no jaundice. They assume the medication is working well-until one day they wake up with yellow eyes or dark urine. By then, the damage may already be advanced.
There’s also a dose effect. Going from 30 mg to 60 mg can double your risk. One 2012 case report documented a patient who developed severe liver injury just two weeks after their dose was increased. That’s not common, but it’s enough to make dose escalation a red flag for monitoring.
Who’s at Highest Risk?
You might think liver damage only happens in heavy drinkers or people with existing liver disease. That’s not true. While those groups are definitely at higher risk, duloxetine can hurt even healthy people.
Studies point to several key risk factors:
- Obesity (BMI ≥30)
- Diabetes
- Regular alcohol use (more than 14 drinks per week for men, 7 for women)
- Taking other medications that stress the liver-like statins, certain antibiotics, or NSAIDs
- Being a poor metabolizer of CYP2D6 (a genetic trait that slows down how fast your body clears the drug)
A 2011 Korean study found three cases of liver injury in Asian patients with no history of alcohol use or liver disease. That case series shattered the myth that only people with preexisting liver problems are at risk. And a 2023 pharmacogenomics study found that people with the CYP2D6 poor metabolizer gene had more than double the risk of liver injury.
What Do Liver Tests Show?
Normal liver function tests (LFTs) include ALT, AST, alkaline phosphatase, and bilirubin. For duloxetine users, the most telling numbers are ALT and AST.
Here’s what doctors look for:
- Mild elevation: ALT or AST 1-3x upper limit of normal (ULN). Often no symptoms. Monitor with repeat testing in 1-2 weeks.
- Moderate elevation: ALT or AST 3-5x ULN. Requires repeat testing within 7 days. Consider holding the drug if levels keep rising.
- Severe elevation: ALT or AST >5x ULN, or any elevation with symptoms like jaundice, nausea, fatigue, or itching. Stop duloxetine immediately.
It’s not just about the numbers. Symptoms matter just as much. If you feel unusually tired, lose your appetite, notice your urine turning dark, or your skin or eyes turning yellow-don’t wait for your next appointment. Call your doctor right away.
How Often Should You Get Tested?
The FDA doesn’t require routine liver testing for duloxetine. But that doesn’t mean you shouldn’t get tested. Major medical societies do.
The American Psychiatric Association and the American Association for the Study of Liver Diseases both recommend:
- Baseline LFTs before starting duloxetine.
- Repeat tests at 8-12 weeks after starting.
- Additional testing at 4 months if you’re high-risk (obese, diabetic, on other liver-affecting meds).
Why 8-12 weeks? Because 78% of significant liver enzyme spikes happen within that window, according to data from 1,247 patients in academic medical centers. After that, the risk drops-but doesn’t disappear. Some cases appear months later.
For patients who’ve been on duloxetine for years without issues, annual LFTs are a reasonable precaution-especially if they gain weight, start drinking more, or begin new medications.
What Happens If Your Liver Is Affected?
If your liver enzymes rise significantly, stopping duloxetine is the first step. In most cases, the liver recovers fully once the drug is out of your system.
One patient on Reddit, who went by ‘AnxietyWarrior42’, had an ALT level of 789 U/L-nearly 20 times the normal limit-after 45 days on 60 mg. He was hospitalized with jaundice. After stopping duloxetine and supportive care, his liver enzymes returned to normal in three months.
On the other hand, ‘ChronicPainSurvivor’ has taken 60 mg daily for five years. Their ALT levels hover between 52 and 68 U/L-slightly above normal but stable and without symptoms. Their doctor monitors them every 3-4 months and considers it safe.
The key difference? Consistent monitoring. One person was caught early. The other was lucky-but also vigilant.
If you need to stop duloxetine, don’t quit cold turkey. Abrupt discontinuation can cause dizziness, nausea, brain zaps, and anxiety spikes. Your doctor should help you taper slowly over 2-4 weeks.
How Does Duloxetine Compare to Other Antidepressants?
Not all antidepressants carry the same liver risk.
Compared to SSRIs like sertraline or escitalopram, duloxetine has about an 80% higher risk of significant ALT elevation, according to a 2019 meta-analysis. Venlafaxine, another SNRI, has a similar risk profile. Tricyclic antidepressants like amitriptyline carry cardiac risks but less liver risk. Bupropion can lower your seizure threshold but rarely affects the liver.
That’s why duloxetine is often avoided in patients with liver disease. The FDA says it’s contraindicated in people with chronic liver disease or cirrhosis. In those patients, duloxetine levels can be up to 7 times higher than normal, making toxicity far more likely.
What Are Patients Saying?
On WebMD, 63% of negative reviews about duloxetine mention unexpected liver side effects. That’s not a small fraction-it’s a loud warning sign.
Many patients say they were never told about liver risks before starting the drug. Others say their doctors didn’t order follow-up tests. One user wrote: "I felt fine. No warning. Then one day I looked in the mirror and my eyes were yellow. I thought I had the flu. Turns out, I almost lost my liver."
Doctors are noticing too. Dr. Sarah Chen, a psychiatrist with eight years of experience, says she’s seen at least three cases of serious transaminitis in her practice-all between day 35 and day 62. All patients recovered fully after stopping the drug.
What’s Changing in 2025?
The field is evolving. In 2023, the FDA released draft guidance pushing for more standardized monitoring of drugs that can cause liver injury-including duloxetine. The American College of Gastroenterology is finalizing new guidelines expected by late 2024, and preliminary drafts suggest recommending baseline liver tests for all SNRI users, not just high-risk patients.
Genetic testing for CYP2D6 status is still experimental, but it’s coming. In the near future, a simple saliva test might tell you if you’re at higher risk before you even start the medication.
Despite the risks, duloxetine remains widely used. In 2023, over 22 million prescriptions were filled in the U.S. alone. Why? Because for many people, it works better than other antidepressants-for depression, yes, but especially for chronic pain. The key is balancing benefit and risk.
What Should You Do?
If you’re on duloxetine:
- Get baseline liver tests before you start, if you haven’t already.
- Ask for a repeat test at 8-12 weeks.
- Know the symptoms of liver trouble: yellow skin/eyes, dark urine, nausea, fatigue, itching, abdominal pain.
- If you’re obese, diabetic, drink alcohol, or take other liver-affecting meds, insist on testing at 4 months.
- Don’t stop the drug suddenly-even if you feel sick. Talk to your doctor about tapering.
If you’re considering duloxetine:
- Ask your doctor: "Will you test my liver before and after I start?" If they say no, ask why.
- Discuss alternatives like SSRIs if you have liver risk factors.
- Be honest about alcohol use, supplements, or other medications.
Duloxetine isn’t dangerous if you’re informed. It’s dangerous if you’re silent.
Can duloxetine cause permanent liver damage?
In almost all cases, liver damage from duloxetine is reversible if caught early. Once the drug is stopped and the liver is given time to heal, enzyme levels return to normal. Permanent damage is extremely rare and usually only occurs if the drug is continued despite severe symptoms and very high enzyme levels. There are no documented cases of liver failure or need for transplant directly caused by duloxetine in otherwise healthy patients.
Are there natural ways to protect my liver while taking duloxetine?
There’s no proven supplement or diet that can prevent duloxetine-related liver injury. Avoiding alcohol, maintaining a healthy weight, and not taking unnecessary medications (like high-dose acetaminophen or certain herbal products) are the best protections. Milk thistle, NAC, or other "liver cleanses" have not been shown to reduce risk in clinical studies. The only reliable protection is regular blood testing and stopping the drug if signs of injury appear.
If my liver enzymes are slightly high, do I have to stop duloxetine?
Not necessarily. If ALT or AST is only 1-3 times the upper limit and you have no symptoms, your doctor may repeat the test in 1-2 weeks. Sometimes, stress, recent illness, or even intense exercise can cause temporary spikes. If the numbers go down or stay stable, you may continue. But if they rise further-especially above 3x ULN-stopping the drug is the safest choice.
Can I switch to another antidepressant if duloxetine affects my liver?
Yes. SSRIs like sertraline, escitalopram, or fluoxetine are generally safer for the liver and are often used as alternatives. Venlafaxine carries a similar liver risk, so it’s not a good substitute. Your doctor can help you transition safely, often by gradually lowering your duloxetine dose while starting the new medication to avoid withdrawal symptoms.
Why doesn’t the FDA require routine liver testing for duloxetine?
The FDA requires labeling about risks but doesn’t mandate monitoring for most medications unless the risk is very high or widespread. Since severe liver injury from duloxetine is rare-about 1 in 10,000 patients-the agency considers it a manageable risk with appropriate clinical judgment. However, professional societies like the American Psychiatric Association and AASLD strongly recommend testing because the consequences of missing it can be serious.


Honestly, this post is overblown. I've been on duloxetine for 7 years. My liver enzymes? Perfect. Doctors don't order tests because the risk is microscopic. Stop fearmongering with case reports.
The data is clear. 1-2% enzyme elevation. 0.6% >3x ULN. You're not a statistic. You're a patient. If your doctor won't test, find one who will. This isn't paranoia-it's due diligence.
I was terrified after reading this but then I talked to my pharmacist. She said if you're healthy, no alcohol, no other meds, just get the baseline test and don't stress. My ALT was 48, normal for me. Keep moving.
In India, many people take this without any monitoring. I know someone who had jaundice after 50 days. He didn't know what was happening until his skin turned yellow. This info could save lives where healthcare access is limited.
i just started duloxetine last week and my liver feels fine?? like i dont even think about it?? but now im paranoid?? like should i drink lemon water?? or just chill??
The FDA doesn't require testing because the incidence is too low to justify population-wide screening. That doesn't mean it's safe. It means the cost-benefit analysis favors clinical judgment over blanket protocols
You people act like duloxetine is poison. I've seen patients on 120 mg for years with normal LFTs. Meanwhile, they're ignoring statins, acetaminophen, and alcohol. Pick your battles
There's a deeper question here. Why do we treat mental health meds like they're disposable? We monitor blood pressure for hypertension, glucose for diabetes. But for depression? 'Just take it and hope.' We've normalized neglect.
Per the American Association for the Study of Liver Diseases, baseline and 8-12 week monitoring is the standard of care for all SNRIs. The FDA's position is regulatory minimalism, not clinical endorsement. Physicians have an ethical obligation to exceed minimums.
I am a psychiatrist who has managed over 400 patients on duloxetine. I have never encountered a case of severe hepatotoxicity. However, I still order baseline and 12-week LFTs-not because I expect harm, but because it demonstrates vigilance and builds trust.
This post is a disaster. Someone's gonna panic and quit their meds cold turkey because of this. What about withdrawal? What about relapse? You're trading one risk for a far more common, far more dangerous one. This isn't medicine. It's anxiety porn.
I’ve been on this for 3 years. My ALT is 55. My doctor says it’s fine. I don’t need a lecture from some internet post. If you’re scared, switch to Zoloft. But don’t guilt people into quitting something that works