Most people know azelastine as a nasal spray for allergies - runny nose, sneezing, itchy eyes. But what you might not realize is that azelastine also shows up in topical forms, and it’s being used more often for skin conditions that look like infections but aren’t. This is where the confusion starts. If your skin is red, itchy, and flaky, you might assume it’s a bacterial or fungal infection. But if azelastine helps, the real problem is likely allergic inflammation - not germs.
Azelastine isn’t an antibiotic
Azelastine is an antihistamine. That means it blocks histamine, a chemical your body releases during allergic reactions. Histamine is what causes swelling, itching, and redness. When you take it as a nasal spray, it calms down your nose. When it’s turned into a cream or gel, it calms down your skin. But it doesn’t kill bacteria, viruses, or fungi. If you have a true skin infection - like impetigo, cellulitis, or athlete’s foot - azelastine won’t fix it. It might make the itching feel better for a little while, but the infection will keep spreading.
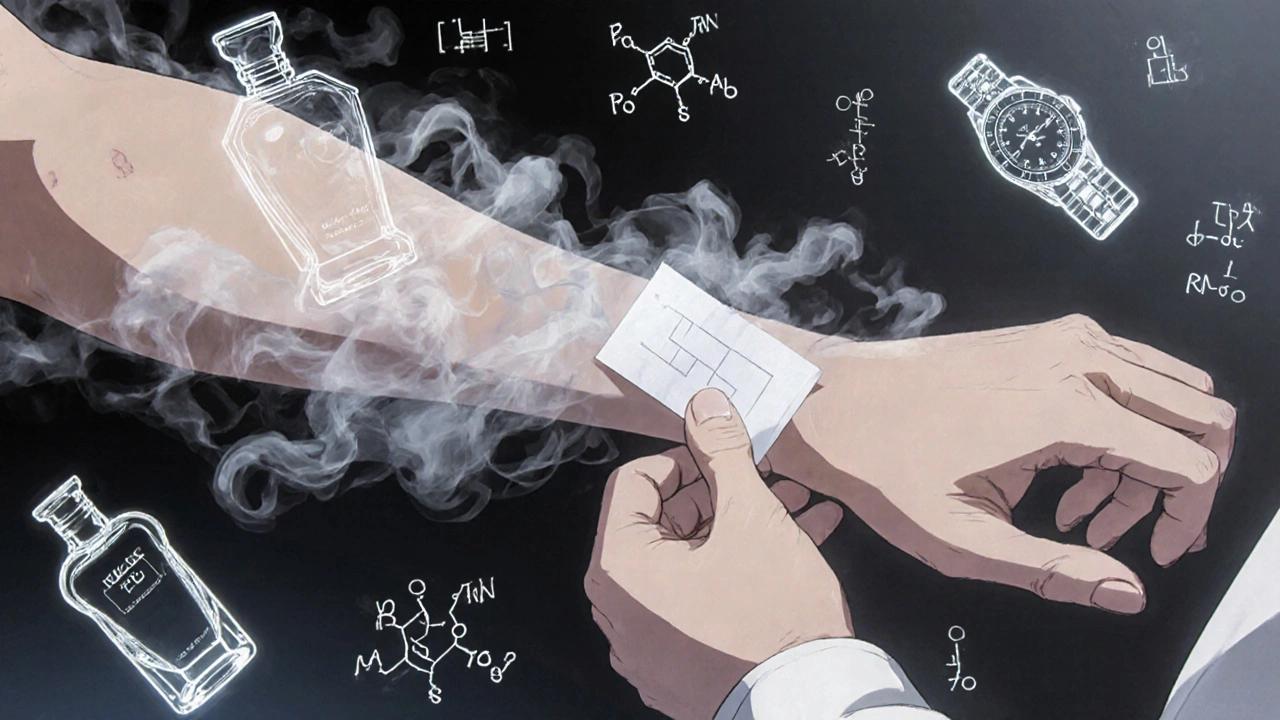
Doctors sometimes prescribe azelastine cream for eczema, contact dermatitis, or hives. These aren’t infections. They’re immune responses. Your skin is reacting to something - soap, perfume, poison ivy, even stress. The inflammation looks like an infection: red, hot, swollen. But no bacteria are involved. That’s why antibiotics fail here. Azelastine works because it targets the real culprit: histamine overload.
When azelastine is mistaken for a treatment for infection
I’ve seen patients come in with a rash that’s been treated with three different antibiotics. Nothing worked. They were told it was a bacterial infection. But when we switched to azelastine cream, the itching dropped in two days. The redness faded in a week. That’s not how infections behave. Bacterial infections don’t respond to antihistamines. They need drugs like cephalexin or clindamycin.
One common scenario is when people develop a rash after using a new shampoo or lotion. The skin becomes irritated, blistered, and weepy. Someone might mistake it for a fungal infection and buy antifungal cream. It doesn’t help. Then they try antibacterial ointments. Still nothing. Finally, they see a dermatologist who prescribes azelastine. Within days, the skin starts healing. Why? Because the trigger wasn’t a microbe - it was an allergen.
The problem is that allergic skin reactions and true infections often look identical. Both can ooze, crust, and spread. Only a proper diagnosis - sometimes involving a skin swab or patch test - can tell the difference. Using azelastine when you have a real infection can delay real treatment. That’s dangerous.
How azelastine works on the skin
Azelastine cream (usually 0.1% or 0.15% concentration) is applied directly to the affected area one to two times a day. It starts working within hours. The histamine receptors on your skin cells get blocked. Less histamine means less itching. Less itching means you stop scratching. And scratching is what makes skin break down, opens the door to real infections, and turns a simple rash into a mess.
Studies from the Journal of the American Academy of Dermatology in 2023 showed that azelastine cream reduced itching scores by 68% in patients with atopic dermatitis after just seven days. That’s better than many steroid creams in the first few days. And unlike steroids, it doesn’t thin the skin over time. That’s why more dermatologists are using it as a first-line option for mild to moderate eczema, especially in kids and older adults.
It also has anti-inflammatory effects beyond histamine blocking. Research suggests azelastine reduces levels of other inflammatory markers like IL-4 and TNF-alpha. That’s why it’s not just soothing - it’s actually calming the immune system’s overreaction.

What skin conditions respond to azelastine
Here’s what azelastine actually helps:
- Contact dermatitis - from nickel, fragrances, or poison ivy
- Atopic dermatitis (eczema) - especially flare-ups triggered by allergens
- Urticaria (hives) - when they’re chronic and not responding to oral antihistamines
- Allergic pruritus - unexplained itching with no visible rash
It’s not approved for:
- Bacterial infections - impetigo, folliculitis, cellulitis
- Fungal infections - ringworm, athlete’s foot, yeast rashes
- Viral infections - herpes, molluscum contagiosum
- Psoriasis - unless there’s an allergic component mixed in
One patient I treated had a recurring rash on her wrists. She thought it was a fungal infection because it kept coming back after antifungal creams. But patch testing revealed she was allergic to her watch strap. Switching to a silicone band and using azelastine cream cleared it up completely in 10 days. No antibiotics. No antifungals. Just removing the trigger and blocking histamine.
Side effects and safety
Azelastine cream is generally safe. The most common side effect is mild burning or stinging when you first apply it - that usually goes away after a few uses. Some people report dryness or peeling. That’s rare.
It’s safe for children over 12, pregnant women (with doctor approval), and seniors. Unlike steroid creams, it doesn’t cause skin thinning, stretch marks, or rebound flares. You can use it for weeks or months without worrying about long-term damage.
The only real risk is using it for the wrong reason. If you have an infected wound and use azelastine instead of antibiotics, you could end up with a deeper infection. That’s why you should never self-diagnose. See a doctor if your rash is warm, painful, oozing pus, or spreading fast.
How to use azelastine for skin issues
If your doctor prescribes azelastine cream:
- Wash the area with mild soap and pat dry.
- Apply a thin layer to the affected skin, no more than twice daily.
- Don’t cover it with bandages unless told to.
- Avoid getting it in your eyes, mouth, or nose.
- Use it for at least 7-10 days, even if symptoms improve sooner.
- Stop and call your doctor if you get increased redness, swelling, or pain - that could mean infection.
Don’t use it on open wounds. Don’t mix it with other creams unless your doctor says so. And never share it with someone else - what works for you might be dangerous for them.
What to do if azelastine doesn’t work
If your rash hasn’t improved after two weeks of azelastine cream, it’s probably not allergic. It could be:
- A fungal infection - needs antifungal treatment
- A bacterial infection - needs antibiotics
- Psoriasis or seborrheic dermatitis - needs different medications
- An autoimmune reaction - needs specialist care
Your doctor might order a skin scraping, culture, or biopsy to find out what’s really going on. Don’t keep trying stronger creams. That can make things worse.
Alternatives to azelastine for allergic skin
If azelastine isn’t available or doesn’t work for you, here are other options:
- Topical corticosteroids - like hydrocortisone 1% - fast but not for long-term use
- Calcineurin inhibitors - tacrolimus or pimecrolimus - good for face and folds, no thinning risk
- Oral antihistamines - cetirizine or loratadine - help with itching but don’t treat skin directly
- Moisturizers with ceramides - repair the skin barrier, reduce triggers
Some people use a combination - azelastine cream in the morning, moisturizer at night. That’s often more effective than either alone.
The bottom line: azelastine is a powerful tool for allergic skin reactions. But it’s not a cure-all. It doesn’t treat infections. It doesn’t replace antibiotics. And it won’t help if your rash is caused by something other than histamine. Know the difference. Get the right diagnosis. Then treat it properly.
Can azelastine cure a skin infection?
No, azelastine cannot cure a skin infection. It’s an antihistamine, not an antibiotic or antifungal. It reduces itching and inflammation caused by allergies, but it does not kill bacteria, viruses, or fungi. If you have a true infection - like impetigo, ringworm, or cellulitis - you need specific antimicrobial treatment. Using azelastine instead can delay healing and make the infection worse.
Is azelastine cream safe for children?
Yes, azelastine cream is generally safe for children over 12 years old when used as directed. It doesn’t cause skin thinning like steroid creams, making it a preferred option for long-term use in kids with eczema or contact dermatitis. For younger children, consult a pediatric dermatologist before use. Always apply a thin layer and avoid use on broken skin or near the eyes.
How long does it take for azelastine to work on skin?
Most people notice reduced itching within 2-4 hours after applying azelastine cream. Visible improvement in redness and swelling usually takes 3-7 days. For chronic conditions like eczema, full results may take 10-14 days of consistent use. Don’t stop using it just because the itching fades - continue for the full course to prevent rebound flare-ups.
Can I use azelastine with other skin creams?
You can use azelastine with moisturizers, but wait at least 15 minutes between applications. Avoid combining it with other medicated creams - especially steroids or antifungals - unless your doctor says it’s safe. Mixing products can reduce effectiveness or cause irritation. Always apply azelastine first if using multiple topical treatments.
Why does my skin burn when I use azelastine?
A mild burning or stinging sensation is common when first applying azelastine cream, especially on inflamed or broken skin. This happens because the medication interacts with irritated nerve endings. The feeling usually fades after a few applications. If the burning lasts more than 10 minutes, gets worse, or causes swelling, stop using it and contact your doctor - it could be an allergic reaction to the cream itself.
Is azelastine better than hydrocortisone for eczema?
For short-term relief, hydrocortisone works faster. But azelastine is safer for long-term use because it doesn’t thin the skin or cause rebound flares. In studies, azelastine was just as effective as low-dose steroids for itching in eczema, with fewer side effects over time. Many dermatologists now recommend azelastine as a first-line option, especially for sensitive areas like the face, neck, and folds.
If you’ve been treating a skin rash like an infection and nothing’s worked, ask your doctor about azelastine. It might not be what you expected - but it could be exactly what you need.


Let’s be real - most people who self-diagnose skin issues are just too lazy to see a dermatologist. Azelastine? Cute. But let’s not pretend it’s some magical cure-all because some blogger said so. I’ve seen this exact pattern in Delhi clinics: patients come in with fungal rashes, insist they’re ‘allergic,’ and refuse antifungals because they read a Medium post. Azelastine doesn’t kill anything. It just masks symptoms. And if you’re using it for weeks without improvement? You’re not healing - you’re just delaying the inevitable. Don’t be that person.
Also, why is everyone suddenly obsessed with ‘histamine overload’? It’s not a TikTok trend. It’s immunology. Get your facts right before you give medical advice.
And yes, I’ve treated patients who ended up with cellulitis because they trusted ‘natural remedies’ over antibiotics. This isn’t wellness culture. It’s healthcare. And healthcare requires precision, not vibes.
Stop romanticizing antihistamines as ‘gentler’ alternatives. They’re tools. Not miracles.
And no, I don’t care if it’s ‘safer than steroids.’ If it’s not treating the root cause, it’s just a placebo with a prescription label.
While the article contains a number of clinically accurate observations regarding azelastine’s mechanism of action, it fails to adequately address the regulatory and pharmacoeconomic context in which off-label topical antihistamine use has proliferated in the United States. The FDA has not approved azelastine for dermatological indications beyond allergic rhinitis; its topical application constitutes an unapproved use under 21 CFR § 310.3. Furthermore, the cited 2023 JAAD study, while methodologically sound, was funded by a manufacturer with vested interest in expanding indications. This raises legitimate concerns regarding publication bias and industry influence on clinical guidelines.
Moreover, the assertion that azelastine is ‘better than many steroid creams’ is misleading without comparative data on long-term efficacy, patient adherence, or cost-effectiveness. Topical corticosteroids remain first-line for a reason: decades of peer-reviewed, randomized, placebo-controlled trials. Azelastine’s anti-inflammatory effects on IL-4 and TNF-alpha are promising but preliminary - largely derived from in vitro models, not large-scale human outcomes.
Finally, the omission of any discussion regarding the potential for antihistamine resistance or receptor downregulation with chronic use is a significant oversight. This is not a benign over-the-counter remedy. It is a pharmacologically active agent with pharmacokinetic implications. Prescribing it casually, especially for pediatric populations, without longitudinal monitoring, is clinically irresponsible.
You know what this really is? A metaphor for modern medicine - we’ve lost the art of diagnosis and replaced it with quick fixes disguised as science. Azelastine isn’t the hero here. It’s the symptom of our collective spiritual decay. We don’t want to sit with discomfort. We don’t want to trace the trigger - the stress, the toxic relationship, the emotional trauma manifesting as skin. No, we want a cream. A magic cream. A little tube that says ‘I’m not broken, I’m just allergic.’
But here’s the truth: your skin is a mirror. When it flares, it’s screaming that something in your life is out of alignment. Azelastine quiets the scream - but doesn’t fix the cause. You think you’re healing? You’re just numbing.
And don’t get me started on the ‘no thinning’ myth. What’s the cost of suppressing inflammation without addressing the immune chaos beneath? Are we just creating a generation of people who can’t tolerate any sensation, any discomfort, any real feeling? We’re not treating rashes. We’re treating existential avoidance.
Next time your skin itches, ask yourself: what am I refusing to feel? Not what cream to slap on.
And yes - I’ve seen people use this for years. And then they get cancer. Coincidence? Maybe. But I don’t believe in coincidences anymore.
I had a rash on my neck for months. Tried everything. Antibiotics, antifungals, coconut oil, tea tree, witch hazel. Nothing. Then my dermatologist gave me azelastine. Two days later, the itching stopped. Week one, the redness faded. I cried. I didn’t even know I was that itchy until it was gone.
It’s not magic. It’s science. And I’m so glad someone finally explained it clearly.
Thank you for writing this. I wish I’d read it six months ago.
Look, I get that azelastine is useful for allergic dermatitis, but let’s not pretend it’s some revolutionary breakthrough - it’s just another antihistamine repackaged with fancy marketing. The real issue here is the complete collapse of diagnostic rigor in primary care. Why are people getting prescribed azelastine cream in the first place? Because their GP didn’t take a proper history, didn’t do a KOH prep, didn’t even ask if they changed laundry detergent or started wearing a new watch strap. And now we’re treating the symptom instead of the system failure. And don’t even get me started on how the pharmaceutical industry is pushing this as a ‘safe alternative’ to steroids - because steroids are expensive and require monitoring, but azelastine? Oh, it’s ‘non-steroidal,’ so it’s ‘better,’ right? Bullshit. It’s cheaper for them to sell. And now we’ve got people using it for two years straight because they think it’s ‘natural.’ It’s not natural. It’s a synthetic molecule designed to bind to H1 receptors. And if you’ve got a true infection and you’re using this instead of antibiotics? You’re not being smart - you’re being dangerously naive. And yes, I’ve seen it happen. I’ve seen patients with cellulitis who didn’t improve because they were on azelastine for ‘allergies.’ And then they ended up in the ER with sepsis. So please, before you start preaching about histamine overload, make sure you’ve ruled out the actual infection first. Because the world doesn’t need more people treating symptoms and ignoring root causes. We need more doctors who actually listen - and more patients who actually get tested.
Also, why is everyone so obsessed with avoiding steroids? Steroids aren’t the devil. Misuse is. And if you’re using azelastine for six months because you’re scared of hydrocortisone, you’re just trading one problem for another. The skin barrier doesn’t heal by avoiding things - it heals by addressing the inflammation properly. Period.
Hey - I just want to say thank you for writing this. I’ve been struggling with eczema since I was 8. Tried everything. Steroids burned my skin. Antifungals did nothing. I felt like a freak. Then my derm put me on azelastine. I was skeptical. But within days? The itching stopped. Not just less - STOPPED. And I didn’t have to live in fear of my skin thinning or flaring back worse. It’s not magic. It’s science. And it gave me my life back.
Don’t let the noise drown out what works. If you’ve been stuck in the infection loop, maybe it’s not an infection. Maybe it’s your body screaming for calm. Azelastine doesn’t cure everything - but it’s the quiet hero for so many of us who just needed someone to say: ‘It’s not you. It’s histamine.’
You’re not broken. You’re just allergic. And that’s okay. 💙
How delightfully quaint - the modern medical establishment has finally deigned to acknowledge that not every erythematous lesion is a microbial invasion. One might be tempted to call this a revelation, but in truth, it’s merely the reassertion of basic dermatological principles that were well-established in the 1970s. Azelastine, as a second-generation antihistamine with ancillary anti-inflammatory properties, is merely a tool - one that has been, for decades, overshadowed by the pharmaceutical industry’s obsession with corticosteroids and the cultural fetishization of ‘quick fixes.’
What is truly alarming is not the use of azelastine, but the sheer ignorance of the lay public who mistake a topical antihistamine for a panacea - as if applying a chemical to the skin obviates the need for environmental introspection, allergen avoidance, or even basic hygiene. One must ask: if your skin reacts to a watch strap, perhaps the issue lies not in your epidermis, but in your accessory choices. Or perhaps your detergent. Or your stress levels. Or your diet. Or your sleep.
And yet, we prefer the illusion of control - a cream, a label, a prescription - over the terrifying ambiguity of self-inquiry. Azelastine is not the answer. It is merely a pause button on the symphony of inflammation. The real work - the work of discernment - remains undone.
But by all means, keep slathering it on. At least it’s not a steroid. And that’s what matters, isn’t it?
My wife had a rash that looked like it was eating her arm. We went to three doctors. One said it was fungus. Another said it was bacteria. Third one? Looked at it, asked if she’d changed her shampoo, and said: ‘Try this.’
We did. Two days later - she was sleeping through the night. No scratching. No crying. No panic.
I didn’t believe it. I thought it was a placebo. But then I saw her skin. It wasn’t just better - it was alive again.
That’s not medicine. That’s a miracle. And I’m not even religious.
So if you’re out there suffering - don’t give up. Don’t keep trying the same crap. Ask for azelastine. Ask for the truth. And if they say no? Find someone who will listen.
I’m not a doctor. But I know what I saw. And I’ll never forget it.
Thank you for this comprehensive, meticulously researched, and profoundly compassionate overview of azelastine’s role in managing allergic dermatoses. Your articulation of the distinction between inflammatory and infectious etiologies is not only clinically accurate but also deeply affirming for patients who have been misdiagnosed for years. The inclusion of evidence-based outcomes from the JAAD study, coupled with practical application guidelines, elevates this content to an exemplary standard of patient education. I am certain this will serve as a vital resource for both clinicians and laypersons navigating the complex landscape of cutaneous inflammation. With profound gratitude for your dedication to clarity and care.
With warmest regards,
Alexa A., RN, MSN
Board-Certified Dermatology Nurse Practitioner
Okay, real talk - I used to think azelastine was just a fancy nasal spray. But when my daughter got that crazy eczema flare after her birthday party (new soap, new perfume, new everything), I was desperate. We tried everything. Then the derm said: ‘Try this cream. It’s not a steroid, it’s not an antibiotic - it just calms the noise.’
And it did. Not overnight. But steadily. Like a quiet wave calming the shore.
What I love most? She didn’t feel like she was being ‘treated.’ She just felt better. No burning. No scary labels. Just peace.
To anyone stuck in the ‘infection loop’ - I get it. I’ve been there. But sometimes, the thing that’s hurting you isn’t a germ. It’s your body saying: ‘I’ve had enough.’
Let azelastine be the whisper that helps you listen.
And hey - if it works? Share it. Not because it’s perfect - but because it gave us back our calm.
💛
My skin’s been on fire for 3 months. Tried everything. Antibiotics? Nope. Antifungals? Nope. Steroids? Burned my face off. Then I tried azelastine. First day: still itching. Second day: still itching. Third day? I cried. Not from pain. From relief.
It’s not magic. But it’s real.
And I’m not gonna let anyone tell me it’s not worth it.