For millions of low-income Americans, the difference between taking a medicine and skipping it comes down to a few dollars at the pharmacy counter. That’s where Medicaid generics make all the difference. In 2023, over 90% of all prescriptions filled through Medicaid were for generic drugs - not because doctors prefer them, but because they work just as well and cost a fraction of the price. For patients living paycheck to paycheck, this isn’t just a policy detail - it’s a lifeline.
Why Generics Are the Backbone of Medicaid
Medicaid doesn’t just cover generic drugs - it relies on them. In fiscal year 2023, generic medications made up 90-91% of all prescriptions paid for by Medicaid, yet they accounted for only about 18% of total drug spending. That’s because generics are priced far lower than brand-name drugs. The average copay for a generic prescription under Medicaid is $6.16. For a brand-name drug? $56.12. That’s nearly nine times more. This isn’t magic. It’s the result of a system designed to stretch taxpayer dollars while keeping care accessible. The Medicaid Drug Rebate Program, created in 1990, forces drugmakers to give states deep discounts in exchange for having their drugs included on Medicaid formularies. For non-specialty generics, Medicaid gets rebates equal to 86% of the retail price. That means if a generic drug retails for $100, Medicaid pays about $14 after the rebate. No other government program gets prices this low.How Much Money Does Medicaid Save?
In 2023, Medicaid rebates cut gross drug spending by $53.7 billion - over half of what would’ve been spent without them. That’s more than the entire annual budget of many U.S. states. The savings don’t just help state budgets. They directly lower out-of-pocket costs for patients. Consider this: 93% of generic prescriptions cost less than $20 at the pharmacy. For brand-name drugs, only 59% fall under that threshold. That’s why a single parent in Texas or a senior in Michigan can refill their blood pressure pill, asthma inhaler, or diabetes medication without choosing between medicine and groceries. The broader impact is staggering. From 2009 to 2019, generic drugs saved the U.S. healthcare system $2.2 trillion. In 2022 alone, generics and biosimilars saved $408 billion. For Medicaid, that means more people can stay on their meds, fewer emergency room visits, and less long-term health damage from untreated conditions.The Hidden Cost: PBMs and Pharmacy Middlemen
Not all savings make it to the patient. Pharmacy Benefit Managers (PBMs) - the middlemen between drugmakers, insurers, and pharmacies - take a cut. A 2025 report from the Ohio Auditor found that PBMs collected 31% in fees on $208 million worth of generic drugs in just one year. That’s over $64 million in fees on drugs meant to be cheap. These fees aren’t always transparent. A patient might pay $6 for a generic, but the state Medicaid program could be paying $15, with $5 going to the PBM and $4 to the pharmacy. The patient never sees that breakdown. That’s why even when generic drug prices drop, some patients still see their copays rise - because PBMs adjust their fees, not because the drug cost changed.
Generics vs. Brand Names: The Real Numbers
Here’s how Medicaid’s generic pricing stacks up against other programs:| Drug Type | Medicaid Average Copay | Commercial Insurance Copay | Uninsured Cash Price |
|---|---|---|---|
| Generic Prescription | $6.16 | $10-$20 | $15-$40 |
| Brand-Name Prescription | $56.12 | $75-$150 | $200+ |
Even compared to Mark Cuban’s Cost Plus Drug Company - which markets itself as a low-cost alternative - Medicaid generics are often cheaper. A 2023 study found that only 11.8% of generic prescriptions would cost less through Mark Cuban’s service than through insurance. For Medicaid patients, the system already delivers the lowest prices.
Challenges: Prior Authorization and Access Delays
Despite the savings, Medicaid patients still face barriers. One major issue is prior authorization. Even for a generic drug, some states require doctors to jump through hoops before the pharmacy can fill it. A Reddit user named MedicaidMom2023 shared that her daughter’s asthma inhaler switched to a generic - cutting her copay from $25 to $3 - but getting approval took three weeks and six phone calls. About 15-20% of Medicaid prescriptions require prior authorization, according to MACPAC. That’s not because the drug is risky - it’s because states are trying to control costs. But delays can lead to skipped doses, worsening conditions, and higher long-term costs. Another problem? Formulary delays. When a new generic hits the market, it can take months - sometimes over a year - for Medicaid to add it to their approved list. During that time, patients may be forced to pay more for an older version or a brand-name alternative.
What’s Changing in 2025?
Medicaid’s drug spending has jumped $10 billion since 2022, reaching $60 billion in net spending in 2024. Why? Not because generics are more expensive - it’s because high-cost specialty drugs are taking up more of the budget. Less than 2% of prescriptions are for drugs costing over $1,000 per claim, but those drugs account for over half of all Medicaid drug spending. In response, the Centers for Medicare & Medicaid Services (CMS) launched the GENEROUS Model in 2024. This initiative focuses on smarter formularies, better use of generics, and cracking down on unnecessary spending on high-cost drugs. It’s not a fix-all, but it’s a step toward making sure savings aren’t eaten up by the most expensive treatments. There’s also talk of extending Medicare’s new drug price negotiation rules to Medicaid. If that happens, experts estimate an extra $15-20 billion in savings over ten years. That could mean even lower copays and fewer coverage denials.What Low-Income Patients Should Know
If you’re on Medicaid, here’s what you need to do:- Always ask if a generic version is available - even if your doctor prescribes a brand name.
- Know your state’s formulary. Each state has a list of covered drugs. You can find it on your state’s Medicaid website.
- Ask about copay tiers. Generics are almost always in the lowest tier - meaning the cheapest price.
- If you’re denied a generic, ask why. It could be a prior authorization issue, not a medical one.
- Don’t assume your pharmacy is giving you the best price. Some pharmacies offer cash prices lower than your copay. Always ask.
Most Medicaid patients don’t need to be experts - the system is designed to work automatically. But knowing how it works helps you push back when something doesn’t add up.

Medicaid generics are one of the most effective social safety nets in the U.S. healthcare system. The data speaks for itself: 90% of prescriptions are generic, yet they consume only 18% of spending. That’s fiscal responsibility without sacrificing health outcomes. Patients aren’t just saving money-they’re staying alive.
It’s not just about cost. It’s about dignity. A single parent in Alabama isn’t choosing between insulin and rent because Medicaid ensures generics are accessible. That’s policy working as intended.
Even when PBMs take their cut, the patient still pays less than they would under commercial insurance. That’s the real win.
Let’s not romanticize the system-it’s flawed, but it’s functional. And for millions, it’s the only thing standing between them and untreated disease.
Advocates should focus on reducing prior authorization delays and increasing formulary transparency-not dismantling what already works.
Okay, but let’s be real-Medicaid’s ‘savings’ are a mirage. PBMs are the real villains here, and you’re glossing over how they manipulate rebates to inflate net costs. The $6.16 copay? That’s not what the state pays. The state pays $15, the PBM pockets $5, and the pharmacy gets $4. The patient sees $6, but the system is rigged.
Also, ‘generics are just as good’? That’s a myth peddled by pharmaceutical lobbyists. Bioequivalence ≠ therapeutic equivalence. I’ve seen patients on generic levothyroxine crash into hypothyroidism because the fill changed from one manufacturer to another.
And don’t get me started on formulary delays. If a new generic hits the market in January, Medicaid might not cover it until October. That’s not efficiency-that’s bureaucratic negligence. 🤦♂️
This is the kind of post that reminds me why I still believe in public programs. 😊
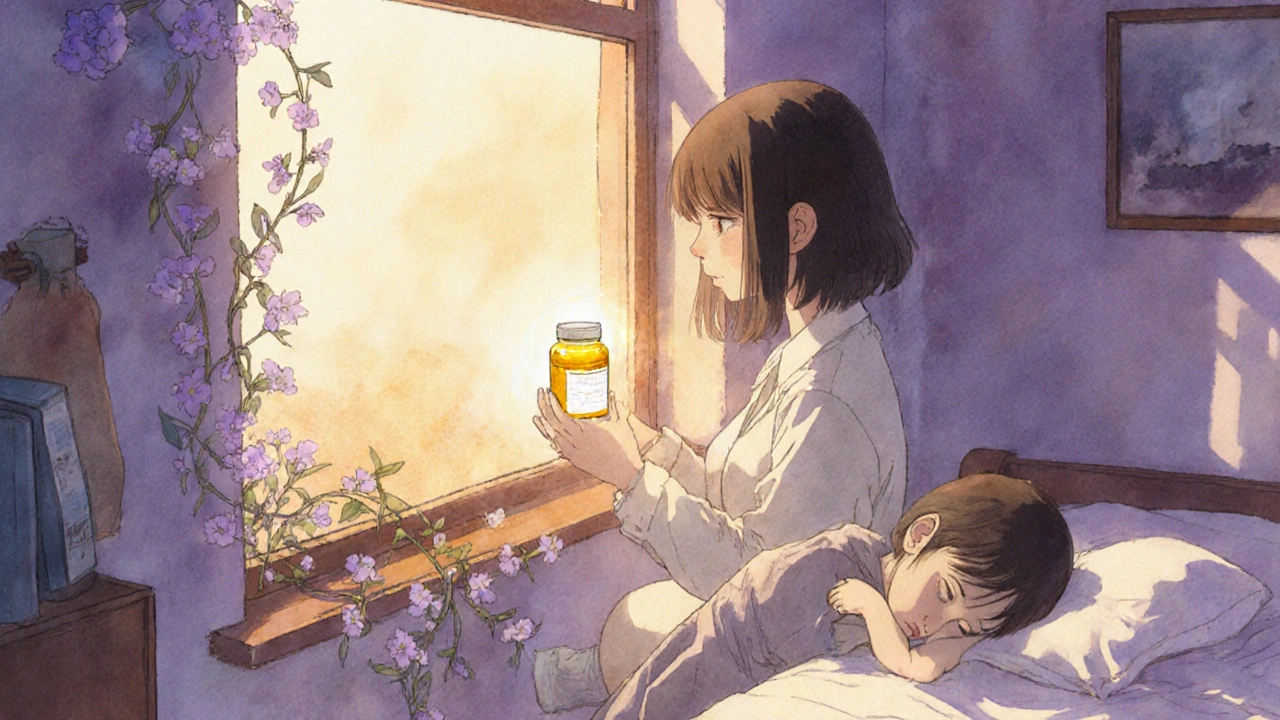
My cousin’s daughter has type 1 diabetes-Medicaid generics let her get insulin without crying every time she checks her bank account. That’s not policy. That’s humanity.
Even if the system’s messy, the fact that a kid in rural Mississippi can get her asthma inhaler for $3 instead of $80? That’s worth fighting for.
Let’s fix the PBMs, sure. But don’t throw out the baby with the bathwater. Generics save lives. Period.
You people are so naive!!! PBMs are stealing from everyone!!! Medicaid patients think they're getting a deal but they're not!!! The state is paying way more than they admit!!! And don't even get me started on how some generics are made in China and have impurities!!! This isn't saving money this is dangerous!!!
While the aggregate data on Medicaid generics is compelling, the structural inequities remain underexamined.
Consider that 15–20% of prescriptions require prior authorization-this creates a de facto rationing mechanism that disproportionately impacts patients with cognitive or linguistic barriers.
Additionally, the claim that generics are ‘just as good’ is statistically misleading. While bioequivalence thresholds are set at 80–125% AUC, clinical outcomes vary by formulation, excipients, and patient metabolism.
And yet, the system incentivizes formulary switching without patient consent. That’s not patient-centered care. That’s cost-shifting disguised as efficiency.
Also: the $2.2 trillion in savings since 2009? That’s not a moral victory. That’s an indictment of a system that only provides care when it’s cheapest-not when it’s optimal.
Let’s stop celebrating austerity as virtue. 💡
Look, I don’t care what the stats say-what matters is that my aunt’s blood pressure meds cost $3 instead of $50. She’s not dying because she couldn’t afford her pills.
Yeah, PBMs are sketchy. Yeah, prior auth is a nightmare. But you don’t fix a broken system by pretending the good parts don’t exist.
Let’s target the middlemen. Let’s speed up formulary updates. Let’s ban gag clauses that stop pharmacists from telling patients they can pay cash for less.
But don’t you dare tell someone who’s taking their meds every day that their lifeline is somehow ‘not enough.’
We can do better. But we can’t start from zero.
One thing the article doesn’t mention: the role of state Medicaid agencies in negotiating bulk pricing with generic manufacturers.
Many states have centralized procurement systems that drive down prices even further than federal rebates alone. For example, California’s Medicaid program negotiates directly with generic makers for 90-day supply contracts, cutting per-unit costs by another 15–20%.
Also, some states now require pharmacies to disclose PBM fees at the point of sale-patients can then choose to pay cash if it’s cheaper. That’s transparency in action.
And while formulary delays are frustrating, many states now have expedited review processes for generics that have been on the market for over a year. It’s not perfect, but progress is happening.
Don’t let the flaws blind you to the fact that this system prevents tens of thousands of ER visits every year. That’s not just savings-it’s saved lives.
Man, this reminds me of how we do it back home in India-generic drugs are the backbone of public health there too. A month’s supply of metformin costs less than a cup of chai. No one bats an eye.
But here’s the thing: in India, you don’t need a PBM or insurance to get it. You walk into a pharmacy, pay cash, and leave. No forms. No prior auth. No drama.
Maybe the real lesson isn’t just that generics work-it’s that when you remove middlemen and bureaucracy, prices drop naturally.
Medicaid’s system is still better than what most of the world has. But we can learn from places that make access simple. Not just cheap. Simple.
generics are just as good lol what a joke i had a friend who took generic adderall and turned into a zombie then switched back to brand and was fine again so stop lying to people
My uncle in Punjab used to say, ‘A good medicine doesn’t need a fancy name.’
He’d walk 3 miles to get his blood pressure pills for 20 rupees-no insurance, no PBM, no prior auth. Just a pharmacist who knew his name and his needs.
Medicaid’s system isn’t perfect, but it’s trying. The real tragedy? In the U.S., we have the tech, the money, the science-and still, we make people fight just to breathe.
Let’s fix the middlemen. Let’s cut the red tape.
But never, ever let anyone tell you that saving lives because it’s cheap is a bad thing.