When your prescription comes back from the pharmacy and it’s not the brand you asked for, it’s not a mistake. It’s generic substitution-a routine part of how insurance works today. Most people don’t realize that 90% of all prescriptions filled in the U.S. are for generic drugs, even though they make up only 18% of total drug spending. That’s because insurers and pharmacy benefit managers (PBMs) push generics hard to cut costs. But what happens when you need the brand? Or when switching causes problems? Here’s how to actually handle insurance requirements for generic substitution without getting stuck with the wrong medicine or a surprise bill.
What Generic Substitution Really Means
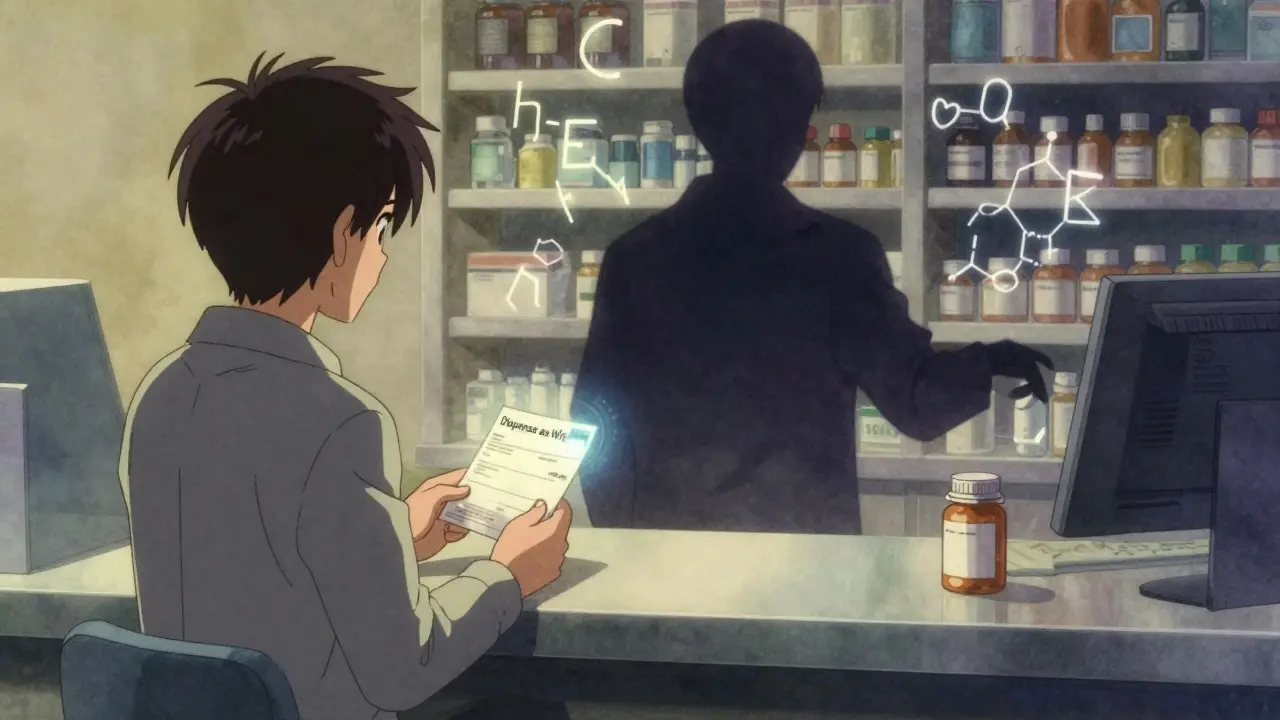
Generic substitution isn’t just a cheaper version of your drug. It’s a legally approved alternative that contains the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. The FDA requires generics to be bioequivalent, meaning they deliver the same amount of medicine into your bloodstream within a tight range-usually 80% to 125% of the brand’s performance. That’s not guesswork. It’s science tested in clinical trials. But here’s the catch: bioequivalence doesn’t mean identical. Generics can have different fillers, dyes, or coatings. For most people, that makes no difference. But for those with sensitivities-say, to lactose or certain dyes-it can cause reactions. One Reddit user reported severe stomach issues after switching from brand-name Synthroid to a generic levothyroxine made by a different manufacturer. The active ingredient was the same, but the inactive ingredients weren’t. That’s not rare. About 24% of complaints on Drugs.com mention inconsistent generic manufacturing.How Insurance Forces Substitution
Your insurance doesn’t just encourage generics-it often mandates them. Most private insurers, like Sun Life and Great West Life in Canada, have policies that pay only for the generic version. If you insist on the brand, you pay the full price difference out of pocket. In the U.S., PBMs like Express Scripts and OptumRx control formularies for 270 million people. If your drug isn’t on their preferred list, you’re either forced to switch or pay more. Some plans use a “mandatory generic” program. That means if your doctor writes a prescription for Lipitor, the pharmacy will automatically fill it with atorvastatin unless you or your doctor says otherwise. If you don’t object, you get the generic. If you do object, you get the brand-but you pay extra. This system is designed to make the generic the default. You have to actively fight to get the brand.When You Can’t Switch-Medical Necessity
Not all drugs are interchangeable. For medications with a narrow therapeutic index-like warfarin, lithium, or certain anti-seizure drugs-tiny changes in blood levels can cause serious side effects. The FDA says approved generics are safe for these drugs, but real-world experience tells a different story. Many doctors and patients report instability after switching. One study found that 30% of patients on levothyroxine needed dose adjustments after switching to a new generic manufacturer. If your doctor believes the brand is medically necessary, they can write “Dispense as Written” or “Brand Medically Necessary” directly on the prescription. In Texas, this is legally binding. In most states, pharmacists must honor it. But not all pharmacists know this. Some still try to substitute anyway. That’s why you need to confirm with them before leaving the pharmacy. For private insurance, you may need to file a prior authorization. That means your doctor submits documentation-like lab results showing your levels went off track after switching, or a history of adverse reactions. Blue Cross Blue Shield of Michigan approves 78% of these requests when proper clinical data is provided. But the process varies. Aetna asks for three criteria. UnitedHealthcare asks for five. If your doctor’s office isn’t used to this, it can take days to get approved.
State Laws Vary-A Lot
There’s no national rule. Every state has its own laws about generic substitution. In 19 states, pharmacists are required to substitute unless told not to. In 7 states and Washington, D.C., they need your written consent before switching. In 31 states, they must notify you-usually on the receipt or label-that a generic was dispensed. But in 24 states, pharmacists have no extra liability if something goes wrong after substitution. Texas has some of the strictest rules. Pharmacists must check the FDA’s “Orange Book” to confirm therapeutic equivalence. They can’t substitute if the doctor wrote “no substitution,” if the patient refuses, or if the generic doesn’t cost the patient less. Even then, they must document everything. If you live in a state that doesn’t require consent, you’re vulnerable. A 2022 survey found that 37% of negative experiences came from patients being switched despite “Dispense as Written” on the script. That’s not just inconvenient-it’s dangerous.What You Can Do to Protect Yourself
You have rights. Here’s how to use them:- Ask your doctor to write “Dispense as Written” or “Brand Medically Necessary” on every prescription if you’ve had issues with generics before. Don’t assume they’ll know to do it.
- Confirm with the pharmacist before you leave. Ask: “Is this the brand I was prescribed? If not, why?”
- Check your receipt. It should say whether a generic was dispensed. If it doesn’t, ask for clarification.
- Know your insurance’s policy. Call your insurer and ask: “Do you require generic substitution? What’s the process to get an exception?”
- Keep a log. If you switch and feel different-more tired, worse symptoms, new side effects-write it down. Note the date, the generic manufacturer, and your symptoms. This is your evidence if you need prior authorization later.
Biologics and Complex Drugs Are Different
Not all generics are created equal. For simple pills, substitution is straightforward. But for complex drugs-like inhalers, injectables, or biologics-it’s not. Biosimilars (the generic version of biologics like Humira or Enbrel) are not identical. They’re “highly similar,” but not the same. The FDA requires extra clinical studies for them. And 45 states now require prescriber notification before substituting a biosimilar. Only 38 biosimilars have been approved in the U.S. as of late 2023, compared to over 10,000 small-molecule generics. If you’re on a biologic, don’t assume substitution is automatic. Your insurer may try to switch you anyway. But under the CARES Act, pharmacists must notify your doctor within five business days if they substitute a biosimilar. That gives your doctor a chance to step in.
Cost Savings Are Real-But So Are Risks
Let’s be clear: generics save money. The average savings per prescription is $327 a year. One user on Reddit saved $45 a month switching from Lipitor to atorvastatin. That’s life-changing for people on fixed incomes. But savings shouldn’t come at the cost of safety. If you’ve had stable control of your condition on a brand, switching for no medical reason is risky. And if you’re one of the 1 in 5 patients who react to inactive ingredients, the savings aren’t worth the side effects. The key is control. You should never be forced to switch without knowing why, without being asked, and without a way to get back to what works. Insurance wants to save money. But your health isn’t a line item.What to Do If You’re Switched Without Consent
If you discover you were switched without your doctor’s approval or your consent:- Call your pharmacy. Ask why the substitution happened. Request the name of the generic manufacturer.
- Contact your doctor immediately. Ask them to write a new prescription with “Dispense as Written.”
- File a complaint with your insurer. Most have a formal appeals process.
- Report the incident to your state’s pharmacy board. Many states track unauthorized substitutions.
Bottom Line: Know Your Rights, Ask Questions, Document Everything
Generic substitution isn’t going away. It’s too cost-effective for insurers. But you don’t have to accept it blindly. You have the right to know what you’re getting. You have the right to refuse. You have the right to ask for the brand if it’s medically necessary. The system works best when you’re informed. Don’t assume your pharmacist or insurance has your best interests at heart. They’re following rules designed to cut costs. Your job is to make sure those rules don’t override your health. Start today: Look at your last prescription. Was it a brand or generic? Did you know? Next time, ask. Document. Speak up. Your body will thank you.Can my pharmacist substitute my brand-name drug without telling me?
In 31 U.S. states and Washington, D.C., pharmacists are required to notify you when they substitute a generic drug. In 19 states, substitution is mandatory unless you or your doctor says no. In 7 states and D.C., they need your explicit consent. If you’re unsure, always ask the pharmacist before leaving the counter.
What does “Dispense as Written” mean on a prescription?
“Dispense as Written” (or “Brand Medically Necessary”) tells the pharmacist not to substitute the brand-name drug with a generic. In most states, pharmacists are legally required to follow this instruction. It’s the strongest tool you and your doctor have to prevent unwanted substitution.
Why do some people have bad reactions to generic drugs?
Generic drugs contain the same active ingredient as the brand, but they can use different inactive ingredients-like fillers, dyes, or coatings. For most people, this doesn’t matter. But for those with allergies, sensitivities, or absorption issues, these differences can cause side effects like stomach upset, rashes, or unstable blood levels. This is especially common with drugs like levothyroxine or seizure medications.
How do I get my insurance to cover a brand-name drug?
Your doctor must submit a prior authorization request with clinical evidence-like lab results showing your condition worsened after switching to a generic, or documented side effects. Most insurers approve these requests if the documentation is solid. Common reasons include therapeutic failure, intolerance, or narrow therapeutic index. Without this, your insurer will only pay for the generic.
Are biosimilars the same as generic drugs?
No. Biosimilars are generic-like versions of complex biologic drugs (like Humira or Enbrel), but they’re not identical. They’re “highly similar” and require more testing than small-molecule generics. Substitution rules are stricter: 45 states require prescriber notification, and 27 require additional patient consent. Never assume a biosimilar is automatically interchangeable.
Can I switch back to my brand-name drug if the generic doesn’t work?
Yes. If you experience side effects or worsening symptoms after switching, contact your doctor immediately. They can write a new prescription with “Dispense as Written” and file a prior authorization for the brand. Many insurers will cover the brand if you can prove the generic didn’t work for you.

Just had this happen last week with my levothyroxine. I switched generics and woke up feeling like I’d been hit by a bus-fatigue, brain fog, heart palpitations. I called my pharmacist. They said, ‘Oh, it’s the same thing.’ No, it’s not. The fillers changed. I had to go back to my doctor, beg for a ‘Dispense as Written,’ and then fight my insurance for three weeks. I’m not exaggerating when I say this saved my life. If you’re on thyroid meds, don’t let them swap it without a fight. Document everything. Even the tiny changes. Your body remembers.
So let me get this straight… I pay $5 for a generic, but if I want the brand, I pay $300… and then the insurance says ‘tough luck’? Yeah, I get it. Save money. But if I’m the one getting sick from the filler, who’s paying for my ER visits? 😒
Biggest thing people miss: pharmacists aren’t required to tell you what manufacturer made the generic. I once got two different generics for the same drug-same name, different pill color, different side effects. Asked the pharmacist. They had no idea. The label just says ‘atorvastatin.’ You gotta ask for the manufacturer name. Write it down. If you get a bad batch, you need to know who made it.
It’s fascinating how a system designed to reduce cost ends up shifting burden onto the patient’s body. We treat medicine like a commodity, but the human body isn’t a spreadsheet. Bioequivalence is a statistical average-not a guarantee for every individual. There’s a philosophical tension here between efficiency and individuality. Who gets to decide what ‘good enough’ means? And why is it always the patient who pays the price when it’s not?
Bro, if you’re on seizure meds or warfarin-DO NOT let them swap. I saw my uncle go into a seizure after switching generics. He was stable for 5 years. One pill change. Boom. Hospital. Doctors said it was the filler. Insurance didn’t care. Now he’s on brand and paying out of pocket. Don’t wait for a crisis. Say no from the start. Your life > their profit.
Generic substitution isn’t evil. It’s capitalism. But the system is broken because it assumes all bodies are the same. They’re not. The FDA’s 80-125% bioequivalence range? That’s a 45% swing. That’s not medicine. That’s a lottery. And if you’re the one who gets the bad draw? You’re on your own. We need mandatory manufacturer labeling on every pill bottle. Not just ‘atorvastatin.’ Name the maker. Who made it. Batch number. That’s basic transparency. Why is that too much to ask?
So the system forces you to fight for your own health. And if you’re tired, broke, or don’t know the lingo? You lose. That’s not healthcare. That’s a maze designed to exhaust you. I’ve seen people give up. I’ve seen people die because they couldn’t afford the brand, and the generic made them sicker. We call this ‘cost-effective.’ I call it cruel.
Imagine if your car’s engine was swapped for a ‘bioequivalent’ version that was 80-125% as powerful. You’d take it back to the dealership screaming. But your body? Nah. Just take the generic. 🤡
Just ask. Always ask. Pharmacist will tell you if it’s generic. If they don’t know, they’re not paying attention. You deserve to know. No shame in asking. Your health is worth it.
While I appreciate the thoroughness of this exposition, I must respectfully assert that the implicit assumption-that patients are passive recipients of pharmaceutical policy-is not only inaccurate but potentially dangerous. Empowerment through knowledge is not a luxury; it is a non-negotiable prerequisite for autonomous healthcare. The onus, therefore, must be placed upon institutions to educate, not upon individuals to survive.
Ugh. I just got switched to a generic and now I’m dizzy. And the pharmacist said ‘it’s the same thing’ like I’m stupid. 🤦♀️ I’m gonna call my senator. This is BS.
For anyone reading this: if you’re on a biologic like Humira, never assume substitution is allowed. Even if your insurer says ‘it’s fine,’ check your state’s law. 45 states require prescriber notification. If they didn’t notify your doctor, it’s a violation. Document the date, the drug, the manufacturer. Then file a complaint with your state board. They hate when people do this. That’s why you should.