Every year, 23,000 people end up in the emergency room because of dangerous mix-ups between supplements and prescription drugs. That’s not a small number-it’s more than the entire population of a mid-sized town. And here’s the scary part: most of these people had no idea their daily vitamin or herbal pill could be quietly canceling out their heart medication, boosting their blood thinners to dangerous levels, or even making their birth control useless.
You take a supplement because you want to feel better, stronger, or healthier. But if you’re also on any kind of prescription medicine-whether it’s for blood pressure, depression, diabetes, or even just a daily aspirin-you’re playing with fire unless you know what you’re mixing.
Why Supplements Aren’t Always Safe with Medications
The idea that "natural" means "safe" is one of the biggest myths in health. St. John’s wort, a popular herb for mood support, doesn’t just gently nudge your system. It can slash the effectiveness of cyclosporine (used after organ transplants) by up to 50%. That means your body might reject the new organ. It can also make birth control pills fail, leading to unplanned pregnancies. And if you’re on an SSRI for depression? Combining it with St. John’s wort can trigger serotonin syndrome-a rare but life-threatening condition that causes high fever, rapid heartbeat, confusion, and seizures.
It’s not just herbs. Even common minerals like calcium, magnesium, and iron compete for the same space in your gut. If you take them at the same time as your thyroid medication or antibiotics, your body absorbs less of the drug. That means your treatment isn’t working as well, even if you’re taking the right dose.
Vitamin E, often taken for skin or immune health, can make blood thinners like warfarin too strong. Studies show doses of 400 IU or higher can push your INR (a blood clotting measure) up by 15-20%. That’s enough to cause internal bleeding without warning.
The Worst Offenders: Supplements That Clash With Drugs
Not all supplements are created equal when it comes to risk. Some are mostly harmless. Others? They’re like chemical grenades in your bloodstream.
- St. John’s wort: The #1 dangerous supplement. It interferes with over 57 medications, including antidepressants, birth control, HIV drugs, and transplant meds. It works by speeding up how your liver breaks down drugs-so they leave your system too fast.
- Ginkgo biloba: Often taken for memory or circulation. Safe for most people. But with blood thinners like Eliquis, Xarelto, or warfarin? It triples your risk of major bleeding. One Reddit user ended up in the hospital for a week after mixing ginkgo with Eliquis.
- Garlic, ginger, and fish oil: These are popular for heart health, but they all thin the blood. Surgeons ask patients to stop them 7-10 days before surgery. Skip this, and you could bleed uncontrollably on the table.
- Goldenseal: Used for colds or digestion. It blocks a key liver enzyme (CYP3A4) that breaks down dozens of drugs. This can cause toxic buildup of medications like statins, leading to muscle damage or kidney failure.
- Vitamin K: If you’re on warfarin, this vitamin directly fights its effect. A sudden increase in vitamin K (from supplements or leafy greens) can make your blood clot when it shouldn’t.
On the flip side, supplements like milk thistle, cranberry, and American ginseng have very few documented interactions. That doesn’t mean they’re 100% safe-but they’re far less likely to cause trouble.
How to Check for Dangerous Mixes (Step by Step)
You don’t need a pharmacy degree to protect yourself. Here’s how to do it right:
- Make a complete list. Write down every pill, capsule, powder, tincture, or tea you take daily-including over-the-counter meds, vitamins, and herbal products. Don’t forget the ones you only take "as needed," like melatonin or magnesium for sleep.
- Bring it all to your doctor or pharmacist. This is called the "brown bag method." You don’t need to explain why you take them. Just hand over the bag. Pharmacists at CVS, Walgreens, and other chains have been trained since 2021 to scan these for interactions. In 18% of cases, they catch something dangerous.
- Ask three specific questions:
- "Does this supplement interact with any of my medications?"
- "Could this affect how well my drug works?"
- "Is there a safer time to take it-like in the morning vs. at night?"
- Check the label. Look for warnings like "Do not take if on blood thinners" or "May interfere with antidepressants." If it’s not there, that doesn’t mean it’s safe. Many labels leave out risks because they’re not legally required to list them.
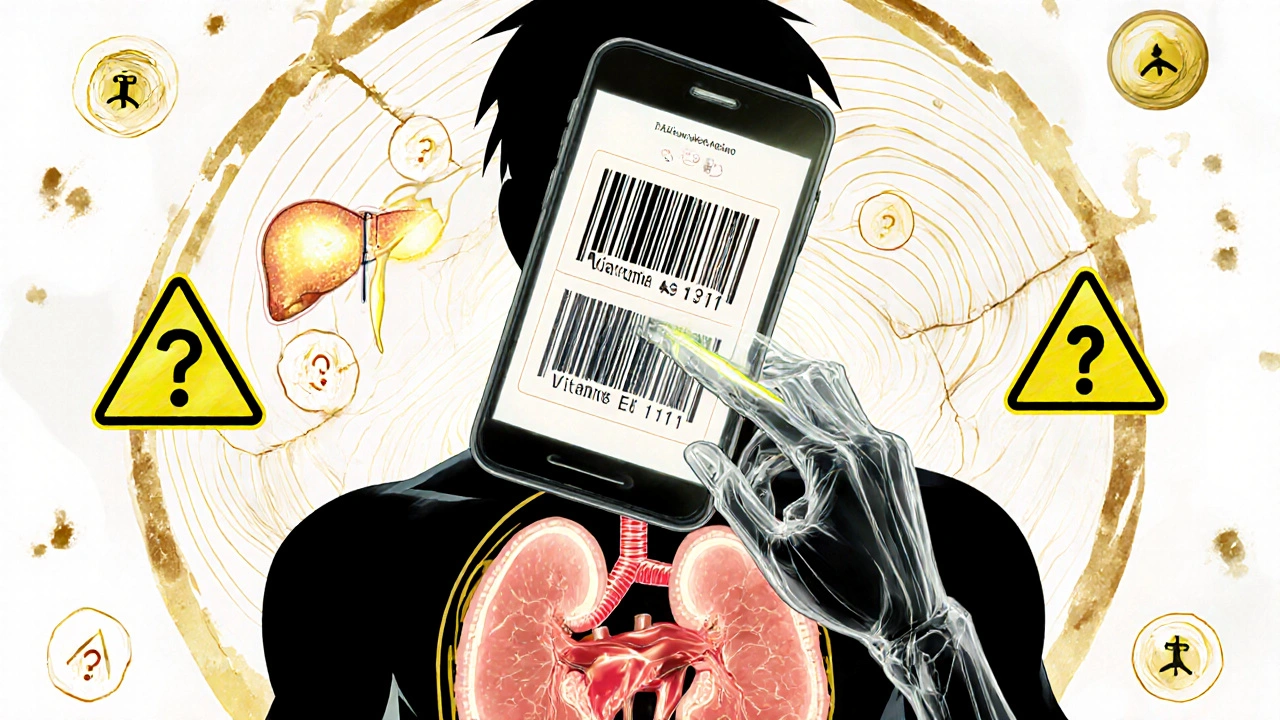
- Use the FDA’s new tool. Starting late 2024, the FDA launched a free mobile app that lets you scan supplement barcodes to instantly check for known drug interactions. It’s not perfect yet, but it’s the first real-time safety tool of its kind.

Who’s at Highest Risk?
If you’re over 50 and taking multiple prescriptions, you’re in the danger zone. Nearly 8 out of 10 adults in this group take both supplements and meds. Yet only 32% ever talk to a doctor about it. Why? Many believe supplements are harmless because they’re "natural." Others think their doctor already knows. They don’t.
Doctors are busy. They don’t ask about supplements unless you bring it up. And even if they do, they might not know the full picture-many aren’t trained in herbal interactions.
People on drugs with a "narrow therapeutic index" are especially vulnerable. These are meds where the difference between a safe dose and a toxic one is tiny. Examples: warfarin, digoxin, cyclosporine, lithium, and thyroid hormones. Even a small change in how your body absorbs or breaks down these drugs can be deadly.
What to Do If You’ve Already Mixed Them
If you’ve been taking a supplement with your medication and you’re not sure if it’s safe:
- Don’t stop your medication cold. Stopping blood pressure or heart meds suddenly can cause a stroke or heart attack.
- Don’t panic. Most interactions don’t cause immediate harm. But they can build up over time.
- Call your pharmacist. They’re the most accessible experts on drug interactions. Most offer free consultations.
- Make an appointment. Tell your doctor you want a medication review. Say: "I’ve been taking [supplement name] and want to make sure it’s okay with my other meds."
What the Experts Say
Dr. Robert Schnoll from the University of Pennsylvania calls St. John’s wort "arguably the most dangerous commonly available supplement." The FDA’s official stance since 2018? "Natural does not equal safe." And the National Institutes of Health’s top supplement researcher, Dr. Josephine Briggs, warns that drugs like warfarin and cyclosporine need "particular caution."
Even Dr. Andrew Weil, a well-known integrative medicine advocate, says St. John’s wort should never be mixed with antidepressants or transplant drugs. He’s not anti-supplement-he just believes in using them wisely.
The Bottom Line: Your Safety Checklist
Here’s what you need to do right now:
- Write down every supplement and medication you take.
- Take your bag to a pharmacist this week.
- Ask: "Could any of these hurt me?"
- Stop taking St. John’s wort, ginkgo, or high-dose vitamin E if you’re on blood thinners or antidepressants-until you get the green light.
- Don’t assume your doctor knows what you’re taking. They probably don’t.
- Use the FDA’s new app when it launches (late 2024).
Supplements aren’t the enemy. But treating them like harmless candy? That’s the mistake that lands people in the ER. You wouldn’t mix cleaning products without reading the labels. Why treat your body any differently?
Can I take vitamin D with my blood pressure medicine?
Yes, vitamin D generally doesn’t interfere with blood pressure medications like lisinopril, metoprolol, or amlodipine. But if you’re also taking calcium supplements or have kidney disease, high doses of vitamin D can raise calcium levels too much, which may affect heart rhythm. Always check with your pharmacist if you’re taking more than 2,000 IU daily.
Is it safe to take melatonin with antidepressants?
Melatonin is usually safe with SSRIs like sertraline or fluoxetine, but it can increase drowsiness. Some studies suggest it might slightly boost serotonin levels, so if you’re on an SSRI and start feeling unusually tired, dizzy, or anxious, talk to your doctor. Avoid high doses (above 5 mg) unless approved.
Why don’t supplement labels warn about drug interactions?
Under the 1994 Dietary Supplement Health and Education Act, supplement makers aren’t required to prove safety before selling their products. They also don’t have to list potential drug interactions on the label. That’s why you can’t rely on the bottle. You need to ask a professional.
Can I just space out my supplement and medication to avoid interactions?
Sometimes, but not always. For example, calcium and thyroid meds should be taken at least 4 hours apart. But with St. John’s wort or ginkgo, spacing won’t help-they change how your body processes drugs over time. The interaction isn’t about timing; it’s about chemistry. Always check with a pharmacist before assuming separation is enough.
What should I do if I experience side effects after starting a supplement?
Stop the supplement immediately. Write down what you took, when you started, and what symptoms you noticed (dizziness, bleeding, nausea, rash, etc.). Call your doctor or pharmacist right away. Report it to the FDA’s MedWatch program at fda.gov/medwatch-it helps track dangerous products. Don’t wait to see if it "goes away." Some reactions get worse.
What’s Next for Supplement Safety?
The FDA is pushing for better labeling and more transparency. By 2027, they aim to cut supplement-related ER visits by 25%. New rules will require clearer warning labels and mandatory reporting of adverse events. Electronic health records are starting to include supplement data-Epic Systems already has it in 15% of U.S. hospitals. And researchers are building AI tools to predict interactions before they happen.
But until then, your best defense is simple: know what you’re taking, talk to your pharmacist, and never assume a supplement is harmless just because it’s on a shelf at the grocery store.


St. John’s wort is a silent killer. I didn’t know it could tank my antidepressants until my psychiatrist caught it during a routine check. I’d been taking it for ‘anxiety’-supposedly ‘natural.’ Turns out, natural doesn’t mean safe. I stopped it cold. My mood stabilized in two weeks. Don’t be me.
Oh honey. You think your ‘immune booster’ is helping? That turmeric capsule you’re chugging with your blood thinner? Congrats-you’re basically prepping your own internal bleeding party. 🎉🩸
I used to think supplements were just fancy vitamins. Then my mom had a near-fatal bleed after mixing ginkgo with warfarin. She didn’t even know they interacted. I now carry a little card in my wallet with everything I take-supplements, OTC, herbs. I hand it to every new provider. It’s not dramatic. It’s survival.
Western medicine is a scam. These ‘interactions’ are engineered by Big Pharma to keep you dependent. Ayurveda and traditional Chinese medicine have been using herbs for millennia without ER visits. You’re being manipulated by corporate fear-mongering. Trust your body, not the FDA’s profit-driven guidelines.
For anyone reading this and feeling overwhelmed-you’re not alone. I started keeping a little notebook: what I take, when, and why. Even if it’s just a magnesium gummy. I bring it to every appointment. My pharmacist now knows me by name. That’s the power of showing up. You don’t need to be perfect. Just consistent.
It is imperative to note that the Dietary Supplement Health and Education Act of 1994, while well-intentioned, has created a regulatory vacuum wherein pharmacological interactions are neither systematically documented nor legally mandated for disclosure. Consequently, consumer autonomy is predicated upon proactive inquiry rather than institutional safeguarding. One must, therefore, exercise epistemic diligence.
You people are so naive. You think a pharmacist will save you? They’re just paid to push pills. The real danger? The fact that your doctor doesn’t even know what’s in your supplements. They don’t test for it. They don’t care. You’re a walking experiment. And the FDA? They’re on the pharmaceutical payroll.
Of course you’re going to die if you take fish oil with warfarin. You’re not a scientist. You’re a person who reads TikTok advice and thinks ‘natural’ means ‘FDA-approved.’ I’ve seen this exact scenario in my ER rotations. You don’t get a second chance when your INR hits 12. Stop being lazy. Ask the question. Or don’t take the supplement. Simple.
Thank you for writing this. I’m a nurse, and I see this every day. Patients come in with 12 supplements and 5 prescriptions, convinced nothing interacts. I don’t judge-I just say, ‘Let’s look at your list together.’ It’s not about fear. It’s about respect-for your body, your meds, and your life. If you’re reading this, take five minutes. Write it down. Bring it in. You’re worth it.