Every year, thousands of people end up in hospitals because of drug reactions that could have been avoided. Not because the medicine was wrong - but because the right information wasn’t written down clearly in their medical records. If you’ve ever said, "I’m allergic to penicillin," without explaining what actually happened, you’re not alone. But that kind of vague note might be putting your life at risk.
Why Specifics Matter More Than You Think
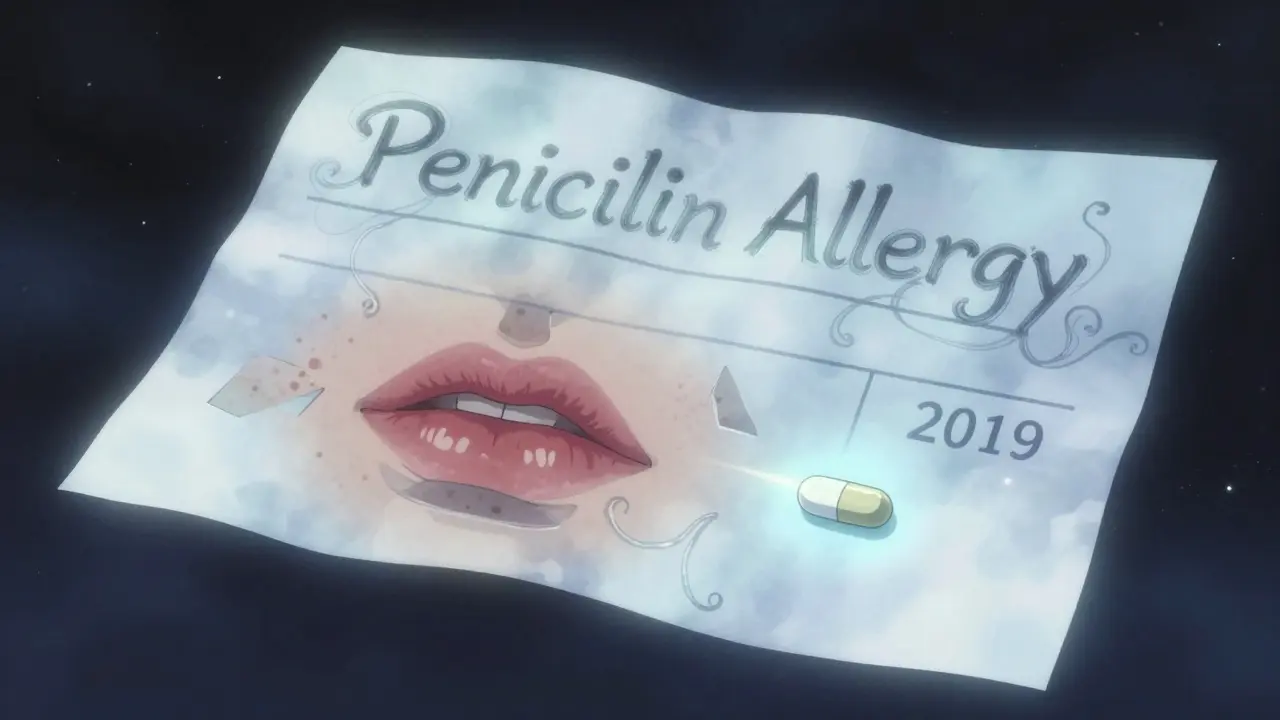
When you tell your doctor, "I’m allergic to sulfa," they don’t know if you broke out in a rash after taking a single pill, or if you went into anaphylactic shock in the ER. That difference changes everything. A rash? Maybe you just had a side effect. Trouble breathing? That’s a true allergy - and it means you can’t get certain antibiotics ever again. The truth is, most people who say they’re allergic to penicillin aren’t. Studies show 90% to 95% of them can safely take it after proper testing. But if your chart just says "penicillin allergy" with no details, your doctor won’t risk it. They’ll pick a stronger, more expensive drug instead - one that might cause more side effects or lead to antibiotic resistance. The key isn’t just saying "I’m allergic." It’s writing down: what drug, what happened, when, and how bad. For example:- Wrong: "Allergic to penicillin"
- Right: "Ampicillin caused hives and swelling of lips in 2019. Reaction resolved with antihistamines. No breathing issues."
What Your Medical Record Must Include
By law, hospitals and clinics in the U.S. must document drug allergies properly. The Centers for Medicare & Medicaid Services (CMS) requires that every patient’s record include:- The exact generic name of the drug (not brand names like "Advil" - say "ibuprofen")
- Specific symptoms (rash, vomiting, low blood pressure, swelling, trouble breathing)
- Severity (mild, moderate, severe, life-threatening)
- Date of the reaction
- Whether you’ve been tested since then
The Hidden Danger of Vague Allergies
A 2018 study at Massachusetts General Hospital reviewed 202 patient records. They found that 61% of them needed major changes after a simple 10-minute interview. Why? Because most entries were too vague:- "Allergic to penicillin" - 36.7% of all allergy entries
- "Sulfa makes me sick" - no details
- "I got a rash once" - no drug named
How to Fix Your Own Records
You don’t have to wait for a hospital visit. Here’s how to take control:- Look at your medical records. Most clinics let you view them online through patient portals. Check the allergy section.
- If it says "penicillin allergy" with no details, schedule a quick visit with your doctor or pharmacist.
- Bring your own notes: What drug? What happened? How long ago? Did you go to the ER? Did you get tested later?
- Ask: "Can we update this to be more specific?"
- Ask if you should be referred to an allergist for testing - especially for penicillin or sulfa drugs.
What Happens If You Don’t Update Your Records?
Outdated or vague allergy info leads to real harm:- Doctors avoid first-line antibiotics - leading to more side effects and higher costs
- Patients get stronger drugs than needed - increasing risk of C. diff infections
- Emergency staff might give you a drug you’re actually not allergic to - and miss the real cause of your symptoms

What You Can Do Right Now
Start today:- Write down every drug you’ve ever reacted to - even if you think it was "just a rash."
- Include the name of the drug (generic, not brand), what happened, and when.
- Call your doctor’s office and ask for a copy of your allergy list.
- Ask if they use a standardized tool like the Drug Allergy History Tool (DAHT) - if not, suggest it.
- Update your records every time you see a new provider, even if you think nothing changed.
Future Changes Coming
By 2025, all certified EHRs in the U.S. will be required to let patients view, edit, and submit their own allergy information directly through apps or portals. The FDA is also testing tools like MyStudies to let people report reactions from their phones. Soon, you might be able to scan a pill bottle and auto-submit the reaction to your record. But until then, it’s still on you to make sure your story is told clearly - in the right words, in the right place.What to Do If You’re Still Unsure
If you’re confused about what counts as a true allergy:- True allergy = immune system response. Symptoms: hives, swelling, wheezing, anaphylaxis.
- Intolerance = side effect. Symptoms: nausea, headache, upset stomach.
- Side effect = expected reaction. Symptoms: drowsiness from antihistamines.
What’s the difference between a drug allergy and a side effect?
A drug allergy is when your immune system reacts to a medication, causing symptoms like hives, swelling, trouble breathing, or anaphylaxis. A side effect is a known, non-immune reaction - like nausea from antibiotics or drowsiness from painkillers. Side effects are common and expected. Allergies are rare and dangerous.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Up to 95% of people who think they’re allergic to penicillin lose the allergy over time - even if it happened decades ago. Testing can confirm whether you still react. Don’t assume you’re still allergic just because you had a reaction once.
Should I carry a medical alert card for drug allergies?
It helps, but it’s not enough. Your medical records must be updated too. Emergency responders might not see your card, but they will check your EHR. Always make sure your doctor has the correct, detailed info - and keep your card updated as well.
Can I be allergic to a drug I’ve taken before without problems?
Yes. Allergies can develop after repeated exposure. You might take a drug safely 10 times - then react on the 11th. That’s why documenting every reaction matters, even if it happened years ago.
What if my doctor won’t update my allergy record?
You have the right to accurate medical records under U.S. law. Ask for a copy, then submit a written request to correct it. If they refuse, contact the clinic’s patient advocate or file a complaint with your state’s medical board. Your safety depends on this being done right.

So basically, if you said 'I'm allergic to penicillin' in 2012 because you got a rash after a tonsillectomy, you're now stuck with antibiotics that give you diarrhea and cost $300 a pill? Cool. Glad we're optimizing for hospital profits over patient comfort.
Also, why is it my job to educate my doctor? I pay taxes for this system. Not to mention the 17 different portals I have to log into just to find my own blood type.
🚨 ALERT 🚨
THEY’RE HIDING THE TRUTH. PENICILLIN ISN’T THE PROBLEM. IT’S THE FILLERS. THE DYES. THE CORPORATE SYNTHETIC ADDITIVES. THEY WANT YOU TO THINK YOU’RE ALLERGIC SO YOU’LL KEEP BUYING THEIR EXPENSIVE ‘SAFE’ DRUGS. 🧪💊
THE FDA IS IN BED WITH BIG PHARMA. CHECK YOUR VACCINE CARDS. THEY’RE LYING ABOUT THE INGREDIENTS TOO. 🤫
Bro, just write it down. Drug + symptom + date. Done.
My aunt thought she was allergic to ibuprofen because her stomach hurt. Turned out she just drank it on an empty stomach. Updated her record. Now she saves $200 every time she gets a headache. 🙌
This isn’t about paperwork. It’s about identity. Your medical record is your body’s autobiography. If you write ‘penicillin allergy’ like a lazy footnote, you’re not just misinforming doctors-you’re erasing your own history.
Think about it: if your diary said ‘I was sad once’ without context, would anyone understand you? No. So why treat your body like a vague tweet?
We’ve turned healthcare into a checklist. But people aren’t checkboxes. They’re stories. And stories need details.
Update your record. Not because the system demands it. Because you deserve to be understood.
And if you’re still scared? Go get tested. You might be free.
-Franklin
It is truly astonishing that, in the 21st century, patients are still expected to act as de facto medical administrators. One would assume that the infrastructure necessary to accurately document and verify clinical data would be both standardized and automated. Alas, we are left to manually correct systemic failures-while simultaneously navigating opaque patient portals and bureaucratic indifference.
How is this acceptable? It is not.
-Nancy
LOL at people who think they’re ‘allergic’ to penicillin because they threw up once in college. That’s not an allergy, that’s bad tequila.
Also, why do we even have these forms? Just give me the drug and let me deal with the side effects. I’m not a fragile snowflake.
PS: I’ve taken 12 antibiotics in 5 years. Never died. You’re all overreacting.
PPS: I still use Advil. Don’t @ me.
😤
Let’s be honest: this entire system is a performative charade designed to absolve clinicians of liability while burdening patients with administrative labor. The fact that you must now become a medical historian to avoid being prescribed a suboptimal antibiotic speaks volumes about the collapse of professional responsibility.
Meanwhile, the EHR vendors are raking in billions because they built a system that requires you to fill out 17 forms just to get a Band-Aid.
And don’t get me started on the ‘No Known Drug Allergies’ checkbox. That’s not documentation-it’s a legal loophole dressed up as diligence.
It’s not your fault. It’s the system.
And the system is broken.
-Jaden
Actually, the post is spot-on-but you missed one key thing: if you say 'allergic to sulfa,' you might be avoiding sulfa-containing diuretics, diabetes meds, or even some eye drops. That’s not just antibiotics-it’s your entire treatment tree.
Also, ‘I got a rash once’ is the worst possible entry. Ever. Ever. Ever.
Update your record. Do it now. I’m not joking. 📝✨
THEY’RE USING YOUR ALLERGY DATA TO TRAIN AI TO PREDICT YOUR HEALTH BEHAVIORS. EVERY TIME YOU SAY ‘ALLERGIC TO PENICILLIN,’ YOU’RE GIVING BIG PHARMA A DATA POINT TO MARK YOU AS ‘HIGH-RISK, LOW-VALUE.’
THEY DON’T WANT YOU TO BE TESTED. THEY WANT YOU TO STAY AFRAID. THEY WANT YOU TO TAKE THE EXPENSIVE DRUGS.
THEY’RE MONITORING PORTAL LOGINS. THEY KNOW WHEN YOU CHECK YOUR RECORDS.
YOUR EHR ISN’T YOURS. IT’S A SURVEILLANCE TOOL.
THEY’LL NEVER TELL YOU THIS.
-ANGEL
Dear Sir/Madam, I am writing to formally request clarification regarding the grammatical structure of the phrase 'sulfa makes me sick.' Is 'sick' a clinical term? Should it be replaced with 'gastrointestinal distress' or 'emesis'? Also, I noticed the post uses American spelling-would British English be acceptable for medical records?
Yours faithfully,
Nidhi Rajpara
WE JUST UPDATED OUR RECORDS!! 🎉
Chris: ‘Amoxicillin → hives, lips swelled, 2021. Antihistamines helped. No ER.’
Kara: ‘NSAIDs → stomach cramps, 2018. Not an allergy. Just sensitive.’
Done in 10 minutes. Now we feel like superheroes. 💪❤️
I never thought about this until my mom got prescribed an antibiotic she couldn’t take-because her chart just said ‘allergic to penicillin.’ She cried. Not because of the drug. Because she’d been avoiding safe meds for 20 years.
So I called her doctor. We updated it. She’s getting tested next month.
It’s not glamorous. But it matters.
-Donna
My grandma thought she was allergic to codeine because she got dizzy. Turns out she just had low blood pressure. She was on pain meds she didn’t need for 15 years.
She’s 82. Took her 3 calls and one appointment to fix it.
Don’t wait. Even if you think it’s ‘no big deal.’
Love you, grandma. 🤍
Interesting. In the UK, we’ve had structured allergy fields in EHRs since 2016. But you still get GPs typing ‘allergic to penicillin’ in free text. Same problem.
It’s not just American. It’s human.
People are lazy. Systems are dumb. We need better training-and maybe a reminder sticker on every computer: ‘DETAILS SAVE LIVES.’
-Jamie
I work in a clinic and we started using the DAHT tool last year. Guess what? Our allergy-related errors dropped 70%.
Patients were way more likely to remember details when asked with a simple form: ‘What drug? What happened? When?’
Doctors don’t need more paperwork. They need better tools.
And patients? They just need to be asked the right way.
-Lisa