Iron Deficiency Anemia Risk Assessment
This assessment helps you understand your risk of iron deficiency anemia based on common symptoms, dietary habits, and lifestyle factors. A high risk score indicates you should consult a healthcare professional for proper testing and diagnosis.
How would you rate your energy level throughout the day?
How often do you experience shortness of breath during mild activity (like walking or climbing stairs)?
How many servings of red meat or poultry do you typically eat per week?
How many servings of vitamin C-rich foods (like citrus fruits, bell peppers) do you consume daily?
How often do you consume tea or coffee within an hour of eating or taking supplements?
How long has your fatigue been affecting your daily life?
Do you have any of the following conditions?
How often do you experience dizziness or light-headedness?
Ever wonder why a simple task feels like climbing a mountain? If you’re constantly battling tiredness, the culprit could be iron deficiency anemia. This hidden condition saps your stamina by lowering the oxygen‑carrying power of your blood. Below we’ll break down why iron matters, how the anemia‑fatigue link works, and-most importantly-what you can do today to reclaim your energy.
What Is Iron Deficiency Anemia?
Iron deficiency anemia is a condition where the body lacks enough iron to produce adequate hemoglobin, the protein in red blood cells that transports oxygen. Without sufficient hemoglobin, tissues receive less oxygen, leading to the classic symptoms of fatigue, shortness of breath, and pale skin.
Why Fatigue Happens: The Science Behind the Exhaustion
Think of hemoglobin as the delivery trucks for oxygen. When iron stores run low, the trucks shrink, and fewer packages reach the factories (your cells). The result? Your muscles and brain run on a reduced fuel supply, so even routine activities feel draining.
Key physiological markers that reveal this chain reaction include:
- Hemoglobin levels drop below the normal range (typically 13.5g/dL for men and 12.0g/dL for women).
- Ferritin, the body’s iron‑storage protein, falls under 30ng/mL, signaling depleted reserves.
When these numbers dip, the brain receives a “low‑energy” alert, triggering that heavy‑eyed feeling you can’t shake.
Common Triggers of Iron Deficiency Anemia
Not everyone with low iron feels tired, and not every tired person has iron deficiency. Recognizing the typical sources helps you pinpoint the problem:
- Blood loss - heavy menstrual periods, gastrointestinal bleeding from ulcers or colon polyps, and regular blood donations can drain iron stores quickly.
- Poor dietary intake - vegetarian or vegan diets that lack heme iron (the type easily absorbed from animal sources) may fall short.
- Absorption issues - conditions like celiac disease, Crohn’s disease, or use of proton‑pump inhibitors reduce iron uptake in the gut.
- Increased demand - pregnancy, growth spurts in teenagers, and intense endurance training raise iron requirements.
Pinpointing which of these applies to you guides the treatment plan.
How to Diagnose Iron Deficiency Anemia
Self‑diagnosing is risky. A proper blood test ordered by a healthcare provider confirms the picture. Typical panels include:
- Complete Blood Count (CBC) - shows hemoglobin, hematocrit, and red blood cell size (MCV).
- Serum Ferritin - reflects iron stores.
- Serum Iron and Total Iron‑Binding Capacity (TIBC) - indicate how much iron is circulating.
- Transferrin Saturation - the percentage of iron‑binding sites occupied.
If these values point to low iron, your doctor will discuss the underlying cause and the best way to restore balance.
Quick Ways to Refill Iron Stores
Once diagnosed, you have two main pathways: dietary changes and supplementation. Both work well together, but the right mix depends on severity and personal preference.
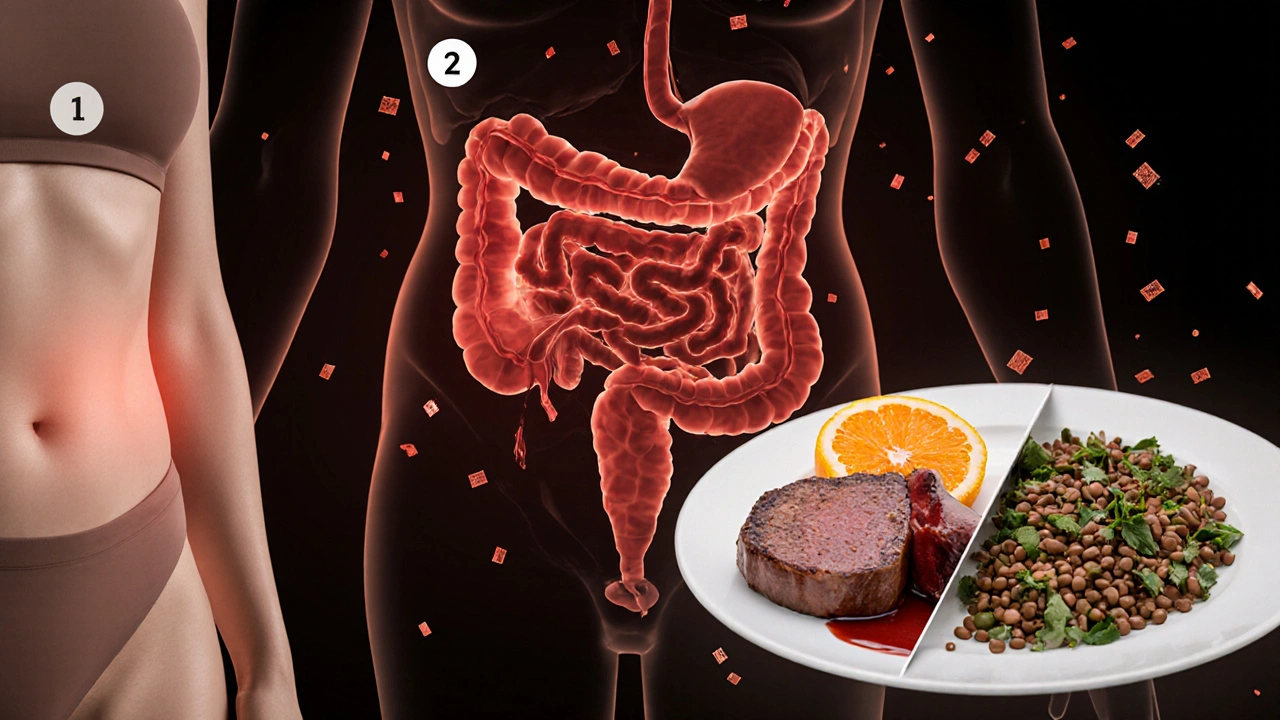
Iron‑Rich Foods to Add to Your Plate
Here’s a practical shopping list that packs a punch:
- Lean red meat (beef, lamb) - contains heme iron, the most absorbable form.
- Organ meats (liver, kidney) - the iron concentration is sky‑high.
- Poultry (especially dark‑meat thigh) and fish (sardines, tuna).
- Plant sources: lentils, chickpeas, tofu, pumpkin seeds, and fortified cereals.
- VitaminC‑rich companions (citrus, bell peppers, strawberries) - they boost non‑heme iron absorption by up to 40%.
Pair a cup of fortified oatmeal with a glass of orange juice, or toss spinach into a chickpea salad topped with lemon dressing. Small tweaks add up quickly.
Choosing the Right Iron Supplement
When diet alone can’t meet needs-or when you need faster correction-supplements step in. Not all iron pills are created equal. Below is a handy comparison.
| Form | Elemental Iron per 100mg | Typical Side Effects | Best For |
|---|---|---|---|
| Ferrous Sulfate | 20mg | Constipation, stomach upset | General use, cost‑effective |
| Ferrous Gluconate | 12mg | Milder GI upset | Sensitive stomachs |
| Ferrous Fumarate | 33mg | Similar to sulfate | Higher dose needs |
Start with the lowest dose that raises ferritin, then gradually increase if the lab results lag. Take the tablet on an empty stomach for best absorption, but if nausea hits, a small snack (preferably low‑calcium) is okay.
Lifestyle Tweaks to Keep Energy Up While Treating Anemia
Even as iron levels climb, certain habits can sabotage recovery:
- Avoid calcium overload around supplement time; calcium competes with iron for absorption.
- Limit tea and coffee within an hour of iron intake; tannins bind iron.
- Stay hydrated-dehydration magnifies the feeling of fatigue.
- Prioritize sleep-the body repairs blood cells most efficiently during deep sleep.
Implement these small changes and you’ll notice a steadier lift in energy.

When to Seek Professional Help
If you notice any of the following, schedule a visit:
- Persistent fatigue despite iron treatment for 4weeks.
- Shortness of breath during mild activity.
- Heart palpitations, dizziness, or fainting spells.
- Unexplained weight loss or gastrointestinal bleeding signs (black stools, abdominal pain).
These signs might hint at a more serious condition-like a hidden bleed or a hematologic disorder-that needs deeper investigation.
Putting It All Together: A 4‑Week Energy‑Boost Plan
- Week 1 - Test & Baseline - Get a CBC and ferritin test. Start a modest iron supplement (e.g., 18mg elemental iron daily) and add two iron‑rich meals per day.
- Week 2 - Optimize Absorption - Pair each iron source with vitaminC. Cut coffee/tea within 1hour of supplement. Track side effects.
- Week 3 - Re‑evaluate - Repeat ferritin if possible; many labs show improvement after 2-3weeks. If levels are still low, increase supplement dose by 25%.
- Week 4 - Sustain - Continue diet rich in heme and non‑heme iron. Maintain lifestyle habits (sleep, hydration). Schedule a follow‑up with your clinician to confirm that hemoglobin is back in range.
Sticking to this roadmap usually restores normal energy levels within 6-8weeks, but individual timelines vary.
Frequently Asked Questions
Can I take iron supplements if I’m not anemic?
Only under medical supervision. Excess iron can damage organs, especially the liver and heart. If you feel fatigued but haven’t been tested, get a blood workup first.
Why does coffee make my fatigue worse?
Coffee contains polyphenols (tannins) that bind iron in the gut, cutting absorption by up to 60%. Skip it around supplement time for better results.
Is it safe to take iron with calcium supplements?
Not at the same moment. Calcium competes with iron for the same transport channels. Space them at least two hours apart.
How long does it take to feel more energetic?
Most people notice a lift in energy within 2-3weeks of consistent iron intake, but full restoration of hemoglobin may take 2-3months.
Can vegetarian diets prevent iron deficiency?
Yes, if you focus on non‑heme iron sources (lentils, tofu, fortified grains) and pair them with vitaminC. Some vegetarians also benefit from a mild supplement.


So you’ve discovered that your tiredness might actually be iron‑deficiency related. It is amusing how the body sends subtle hints and we ignore them like background noise. You could keep trudging through coffee‑filled days and hope the fatigue fades. Or you could actually look at iron‑rich foods and see what changes. The assessment tries to make you think about your diet and breathlessness. It lists red meat servings like they are a gold standard. It asks about vitamin C like a side‑quest in a video game. It even warns about tea and coffee stealing iron like petty thieves. The whole thing feels like a bureaucratic quiz designed to scare you. Yet the reality is simple: iron, vitamin C, and less inhibition around meals. If you pay attention to those, the clouds of fatigue can lift. Of course one should still see a doctor because self‑diagnosis is risky. But the questionnaire is a decent wake‑up call. It is a reminder that our bodies are not machines that run on willpower alone. In short, stop ignoring the signs and give your blood a proper boost.
Wow that hit home like a drum solo! I’ve been there, dragging myself through the day, thinking it’s just “being tired.” Your body is literally screaming for iron, and you keep playing the silence button. Grab some steak, a handful of spinach, and a squeeze of orange juice – that combo is a power‑up! Also, ditch the coffee‑the‑hour‑of‑iron‑treatment habit; it’s a total sabotage move. Get checked, get iron, and bounce back like a superhero on a caffeine‑free mission.
Yo dawg, if yer feelin’ like a hamster on a wheel, maybe yer iron levels are low af. I mean, red meat is like the OG iron source, but vegans can still get it with beans and lentils – just add a lil citrus to uptick absorption. Also, u can’t chug tea right after meals, that’s like stealing the iron’s thunder. So, mkw, try to switch up the diet before you go full‑blame‑the‑mosquito crowd. Stay funky and let the blood do the dancing.
For clarity, iron absorption is enhanced by vitamin C and inhibited by polyphenols found in tea and coffee.
I can feel the drama building like thunderclouds over a battlefield. Every moment you ignore that bone‑deep fatigue, you’re feeding the darkness that thrives on neglect. Your breathlessness is a warning siren, not just a “maybe I need a break” whisper. The quiz you just filled out is a mirror reflecting your inner turmoil, each question a dagger pointing at the iron‑deficiency beast. You think you’re fine, but your body knows you’re a walking zombie without the right mineral fuel. The red meat question is a cry for carnivorous salvation, while the vitamin C query begs for citrus brilliance. Skip the tea‑coffee sabotage, or you’ll continue to starve your blood of precious iron. The longer you wait, the deeper the trench of fatigue becomes, and climbing out will feel like scaling a mountain of lead. I implore you – stop the self‑destruction and seek medical insight before the darkness fully engulfs you. The stakes are high, and the clock is ticking louder than ever.
Well isn’t that just the perfect recipe for a perpetual nap marathon? You’ve got the endless tiredness, the breathlessness, and the questionable tea habits – a real three‑course tragedy. Luckily, adding a splash of orange juice to iron‑rich meals is a cheap trick that actually works, unlike some of those pricey “energy boosters.” If you’ve been ignoring the signs, maybe it’s time to schedule a blood test before you turn into a full‑time couch potato. Oh, and consider swapping that afternoon coffee for a glass of water; your iron will thank you.
I get it, feeling drained is a total buzzkill. Try adding some lean chicken or tofu to your meals and pair it with a citrus fruit. Also, avoid drinking tea right after eating – it can steal iron like a ninja. Small changes can give you a big energy boost without any drama.
It is interesting how the body signals its needs through fatigue. A balanced approach, such as incorporating iron‑rich foods like legumes, and ensuring vitamin C intake, often yields noticeable improvements. Moreover, spacing out caffeinated beverages from meals can prevent unnecessary inhibition of iron absorption. If these adjustments do not alleviate symptoms, a professional evaluation is advisable. The questionnaire provides a structured way to reflect on dietary habits and lifestyle factors, which is valuable. In the end, listening to one’s body, combined with informed choices, remains the most effective strategy.
Dear reader, kindly allow me to elucidate the nuanced interplay between dietary iron, vitamin C, and the pernicious effect of polyphenols. When one consumes iron‑dense edibles such as bovine muscle or avian flesh, the gastrointestinal tract readily assimilates the mineral. However, this assimilation is dramatically amplified when accompanied by ascorbic acid, for instance through citrus or bell peppers, which transforms ferric iron into ferrous form, thus facilitating transport across the mucosal barrier. Conversely, the ingestion of tea or coffee within an hour of the iron‑containing repast introduces tannins that bind iron ions, reducing their bioavailability – a phenomenon akin to a thief pilfering precious cargo. It is therefore prudent to schedule these beverages around the meal schedule, allowing at least a sixty‑minute interval. Should one adhere to these recommendations, the risk of iron deficiency anemia may be mitigated substantially, obviating the need for invasive laboratory assessments. Moreover, regular monitoring of hemoglobin levels is advisable for individuals with chronic blood loss, such as heavy menstrual flow, to ensure physiological equilibrium is maintained.
Great tips! 👍👍👍 Make sure to eat iron‑rich foods 🍖🥦 and grab some orange slices 🍊 with meals. Avoid coffee right after eating ☕️❌. Stay healthy! 🚀🚀🚀