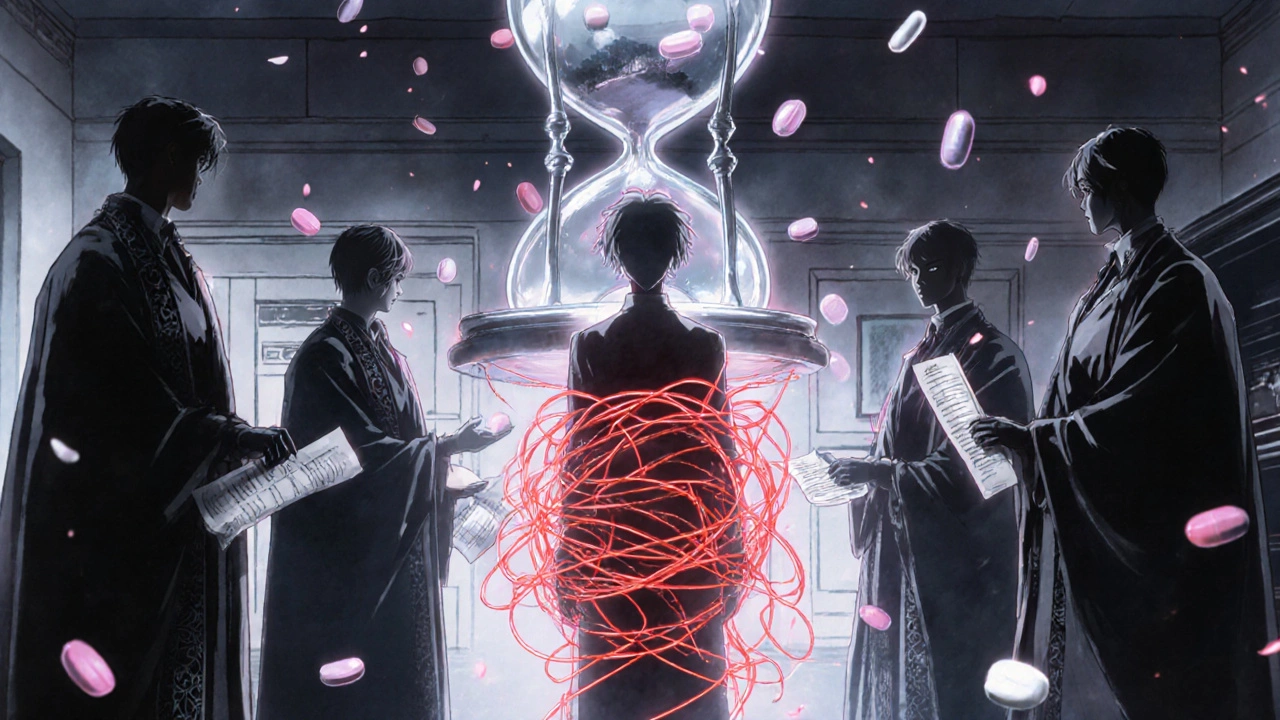
Taking five or more medications a day isn’t unusual - especially for older adults or people managing several chronic conditions. But the more pills you take, the higher the chance something will go wrong. Drug interactions, side effects, and confusion can turn a treatment plan into a health risk. The truth is, polypharmacy - the regular use of five or more medications - isn’t always bad. But when it’s not managed carefully, it becomes dangerous.
Why Polypharmacy Happens
Polypharmacy doesn’t happen overnight. It builds up over time. Someone starts with one medication for high blood pressure. Then they develop diabetes and get another pill. A knee problem leads to painkillers. Insomnia brings in sleep aids. Over-the-counter supplements get added because they’re ‘natural.’ And before long, the medicine cabinet looks like a pharmacy shelf. It’s not just patients’ fault. Care fragmentation plays a big role. One doctor treats your heart, another handles your joints, and a third manages your mental health. None of them talk to each other. Each prescribes what they think is best - without seeing the full picture. That’s how prescribing cascades happen: a side effect from one drug gets treated with another drug, which causes a new side effect, and so on. And then there’s the problem of not stopping what’s no longer needed. A medication prescribed for a short-term infection might still be on the list five years later. Or a cholesterol drug might have been useful ten years ago, but now your health goals have changed. Yet no one ever asked if it’s still necessary.What Makes a Medication Unsafe in a Polypharmacy Regimen
Not all multiple medications are harmful. The key difference is between appropriate and inappropriate polypharmacy. Appropriate polypharmacy means every drug has a clear purpose, is backed by evidence, matches your health goals, and is something you can actually take consistently. For example, someone with heart disease, diabetes, and high blood pressure might need three or four medications - and that’s fine if they’re working together and you’re not having side effects. Inappropriate polypharmacy is when:- A drug has no valid reason to be taken anymore
- The risks outweigh the benefits
- The medication causes side effects that make you feel worse
- You’re taking it but not following the schedule because it’s too complicated
- You’re using it to treat a side effect of another drug
The Five-Step Safety Framework for Managing Multiple Medications
The World Health Organization outlines a clear, practical way to manage polypharmacy safely. It’s not complicated - it just requires consistency and teamwork.- Review each medication’s purpose - Every pill should be tied to a specific diagnosis. If you can’t name the condition it’s treating, it might not belong on your list.
- Do a full medication review - This isn’t just checking your prescriptions. Include over-the-counter drugs, vitamins, herbal supplements, and even topical creams. A pharmacist can help spot hidden interactions.
- Check for interactions - Some drugs don’t mix well. For example, blood thinners like warfarin can become dangerous if taken with certain antibiotics or even grapefruit juice. Tools like the Beers Criteria or electronic alerts in medical systems help flag these.
- Communicate with your care team - Make sure your primary doctor, pharmacist, and specialists are all on the same page. Bring your full list to every appointment - not just what you think is important.
- Reconcile meds during transitions - When you’re discharged from the hospital, moved to a new care facility, or see a new doctor, your medication list must be double-checked. Mistakes here are one of the most common causes of hospital readmissions.
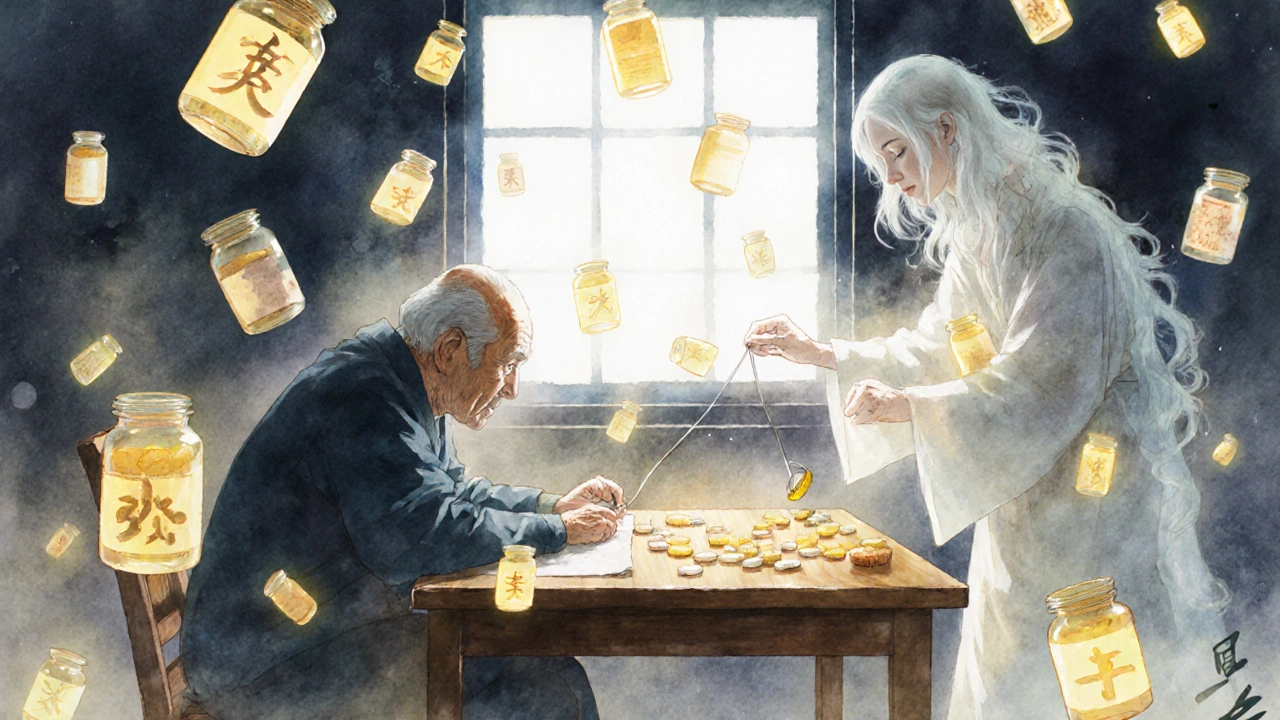
Deprescribing: When Less Is More
Deprescribing isn’t about cutting pills just to reduce numbers. It’s about removing drugs that no longer serve you - safely. Some medications can’t be stopped suddenly. Blood pressure pills, antidepressants, and steroids can cause rebound effects or withdrawal symptoms if discontinued too quickly. That’s why deprescribing must be planned, gradual, and supervised. Start by asking: Is this drug still helping me? If you’re taking a statin for cholesterol but your life expectancy has changed due to other health issues, does it still make sense? If you’re on a painkiller that’s making you dizzy and fall-prone, is the pain really worth the risk? A 2024 study found that the most effective way to deprescribe is through a conversation with your doctor - not a checklist. You need to talk about your goals. Do you want to live longer? Or do you want to feel better, sleep better, and avoid hospital visits? Your priorities shape what stays and what goes.Your Role in Managing Your Medications
You’re not just a patient. You’re the most important member of your care team. Here’s what you can do right now:- Keep a real-time medication list - Write down every pill, supplement, and cream. Include the name, dose, why you take it, who prescribed it, and any special instructions (like ‘take with food’ or ‘avoid grapefruit’). Update it after every doctor visit.
- Use one pharmacy - All your prescriptions filled at the same place means the pharmacist can track interactions you might miss. They’ll flag dangerous combos before you even pick them up.
- Link meds to daily habits - Take your pills after brushing your teeth or with breakfast. Routine reduces missed doses and confusion.
- Report new symptoms - If you feel foggy, dizzy, nauseous, or more tired than usual, don’t assume it’s just aging. It could be a drug reaction.
- Never stop or change a dose without talking to your doctor - Even if you think a pill isn’t helping, stopping it cold could be risky.
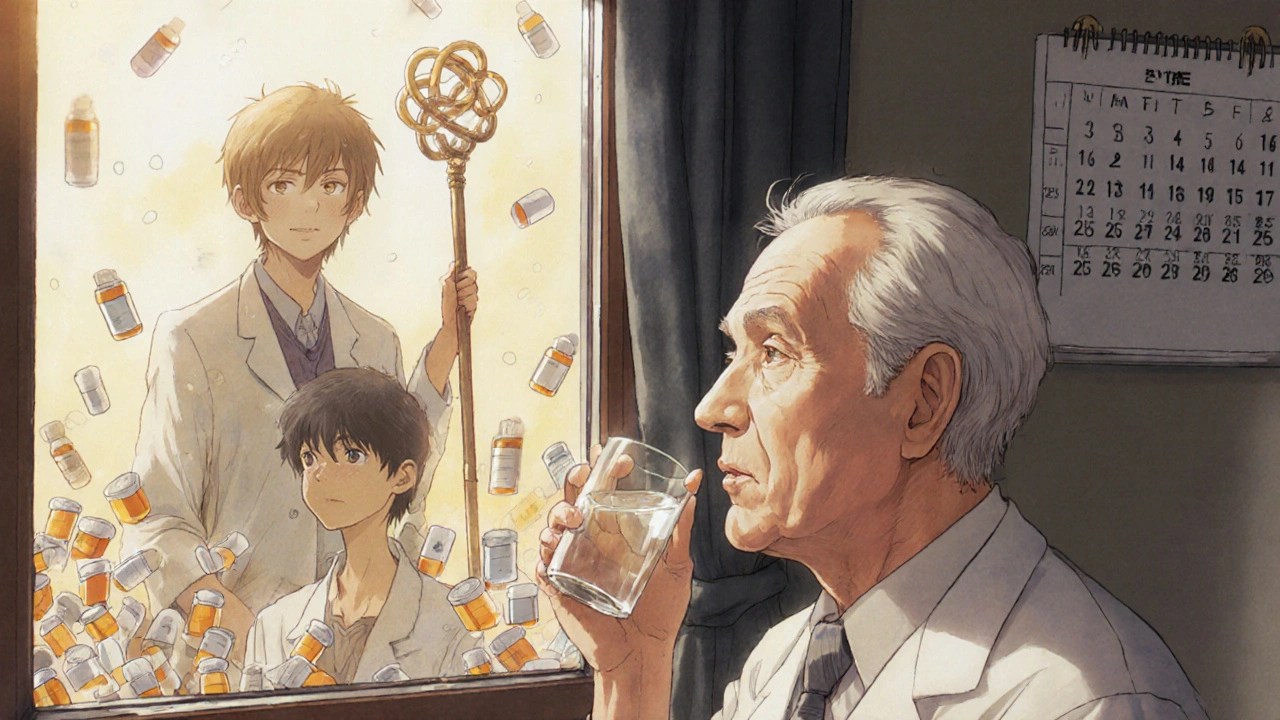
The Team Approach: Why You Need More Than One Doctor
Managing multiple medications isn’t a solo job. It takes a team. Pharmacists are often the unsung heroes here. They’re trained to spot interactions, simplify regimens, and explain what each drug does in plain language. Nurses help track adherence and spot early signs of side effects. Caregivers can remind you to take pills and notice changes in behavior or mood. When care is fragmented - when your cardiologist doesn’t know what your rheumatologist prescribed - mistakes happen. The solution? Structured medication reconciliation at every transition: hospital discharge, clinic visit, or even when switching doctors. Some clinics now have medication therapy management programs where a pharmacist spends 30 minutes with you, reviews your entire list, and works with your doctor to cut or adjust what’s unnecessary. These programs have been shown to reduce hospital visits and improve quality of life.What to Do Next
If you’re taking five or more medications:- Write down every single one - including supplements and OTC drugs.
- Bring that list to your next doctor’s appointment.
- Ask: ‘Is every one of these still necessary? Could anything be stopped or reduced?’
- Ask your pharmacist to check for interactions.
- Set a reminder to review your list every six months - or after any hospital stay.
What is polypharmacy?
Polypharmacy is the regular use of five or more medications at the same time. It’s common in older adults and people with multiple chronic conditions. While sometimes necessary, it increases the risk of drug interactions, side effects, and medication errors if not carefully managed.
Are all multiple medications dangerous?
No. Taking multiple medications isn’t automatically harmful. What matters is whether each drug is still needed, effective, and safe for you. Appropriate polypharmacy means each medication has a clear purpose, matches your health goals, and is taken as directed. Inappropriate polypharmacy includes drugs with no benefit, high risks, or those causing side effects.
How do I know if a medication should be stopped?
Ask yourself: Is this drug still helping me? Does it cause side effects like dizziness, confusion, or fatigue? Is it treating a side effect of another drug? Has your health goal changed? Talk to your doctor or pharmacist. Never stop a medication suddenly - some need to be tapered slowly to avoid withdrawal or rebound effects.
Can supplements interact with prescription drugs?
Yes. Many people assume supplements are safe because they’re ‘natural,’ but that’s not true. St. John’s Wort can reduce the effectiveness of blood thinners and birth control. Garlic and ginkgo can increase bleeding risk with aspirin or warfarin. Always tell your doctor and pharmacist about every supplement you take - even if you think it’s harmless.
Why should I use only one pharmacy?
Using one pharmacy gives your pharmacist a complete picture of all your medications. They can spot dangerous interactions between prescription drugs, over-the-counter products, and supplements. They can also alert you to dosage errors or duplicate prescriptions. This simple step reduces risks significantly.
What is deprescribing?
Deprescribing is the planned, gradual process of stopping medications that are no longer beneficial or are causing more harm than good. It’s not about reducing the number of pills for the sake of it - it’s about improving your safety and quality of life. Deprescribing should always be done under medical supervision.
How often should I review my medications?
Review your medication list at least once every six months - and always after a hospital stay, emergency visit, or change in health. If you’ve seen multiple doctors recently, a full review is essential. Keep your list updated and bring it to every appointment.

Love this breakdown. I’ve been telling my grandma for years to bring her whole pillbox to every appointment-she thought the pharmacist ‘just handed out magic beans.’ Now she’s got a color-coded chart and actually sleeps better. Small wins.
Of course the government and Big Pharma want you to stay on 12 pills a day-more profit, less accountability. They don’t want you to heal. They want you dependent. The ‘Beers Criteria’? Just a PR stunt to make you feel safe while they quietly replace everything with cheaper generics that cause more falls. Ask yourself: Who benefits?
Let’s not romanticize deprescribing as some noble act of liberation-it’s often a cost-cutting measure disguised as patient empowerment. I’ve seen elderly patients quietly have their antihypertensives yanked because their Medicare cap was reached. The ‘team approach’ sounds lovely until the pharmacist is overworked and the doctor hasn’t read the chart since 2021. Transparency is the exception, not the rule.
Why do we even bother? Americans take too many pills. End of story.
Medication is not a moral act. It is a physiological negotiation between chemical structure and biological entropy. To ask if a pill is still necessary is to assume intentionality where there is only inertia. The body does not care about your goals. It responds to molecules. The rest is narrative.
THIS. THIS RIGHT HERE. I was on 17 medications after my triple bypass-felt like a walking pharmacy. Then my pharmacist sat me down for 45 minutes, asked me what I wanted my life to look like-not just how long I wanted to live-and we cut 8 pills. I started hiking again. I cried. This isn’t medicine. This is liberation.
Umm actually in india we dont even get half these meds n most ppl take ayurvedic stuff which is way safer than these chemical bombs. Why are u all so obsessed with pills? Maybe ur system is broken not ur meds.
My mom’s on 9 meds. She forgets half of them. We started using a pill organizer with alarms. She’s been stable for 8 months. No drama. Just consistency.
Deprescribing requires trust. And trust is scarce when your PCP sees you for 7 minutes every 6 months. But when a pharmacist takes the time to explain why a statin might no longer align with your goals? That’s the kind of care that heals. We need more of this.
Just had my first med review with my pharmacist-turned out I’d been taking a blood pressure pill for 7 years after my BP normalized. She laughed, I cried. We took it off. I feel lighter. Not just physically. Mentally too. You don’t need a prescription to feel free.
Big Pharma + FDA = cartel. 🧪💊 They want you addicted. The ‘Beers Criteria’? A placebo for guilt. Your doctor won’t tell you this, but 70% of geriatric meds are just profit-driven. Check your insurance formulary. It’s not about safety. It’s about cost.
I’m a caregiver for my dad. He’s on 11 meds. We started tracking them in a shared Google Doc-doses, times, side effects. His neurologist was shocked at how much we knew. Turns out, when you show up prepared, doctors actually listen. It’s not magic. It’s just doing the work they’re too busy to do.