Scaly Skin Diagnostic Tool
This tool helps identify the most likely cause of scaly skin by analyzing your symptoms. Based on the article content, it identifies common conditions and provides guidance on next steps.
When your skin starts developing Scaly Overgrowths of Skin a condition where the outer layer thickens and flakes, often looking dry or crusty, it usually signals an underlying issue. You might think it’s just “dry skin,” but the patterns, location, and accompanying sensations can tell a very different story. This guide walks you through the most common culprits, shows how to read the clues on your own body, and lets you know when professional help is the next step.
What Makes Skin Turn Scaly?
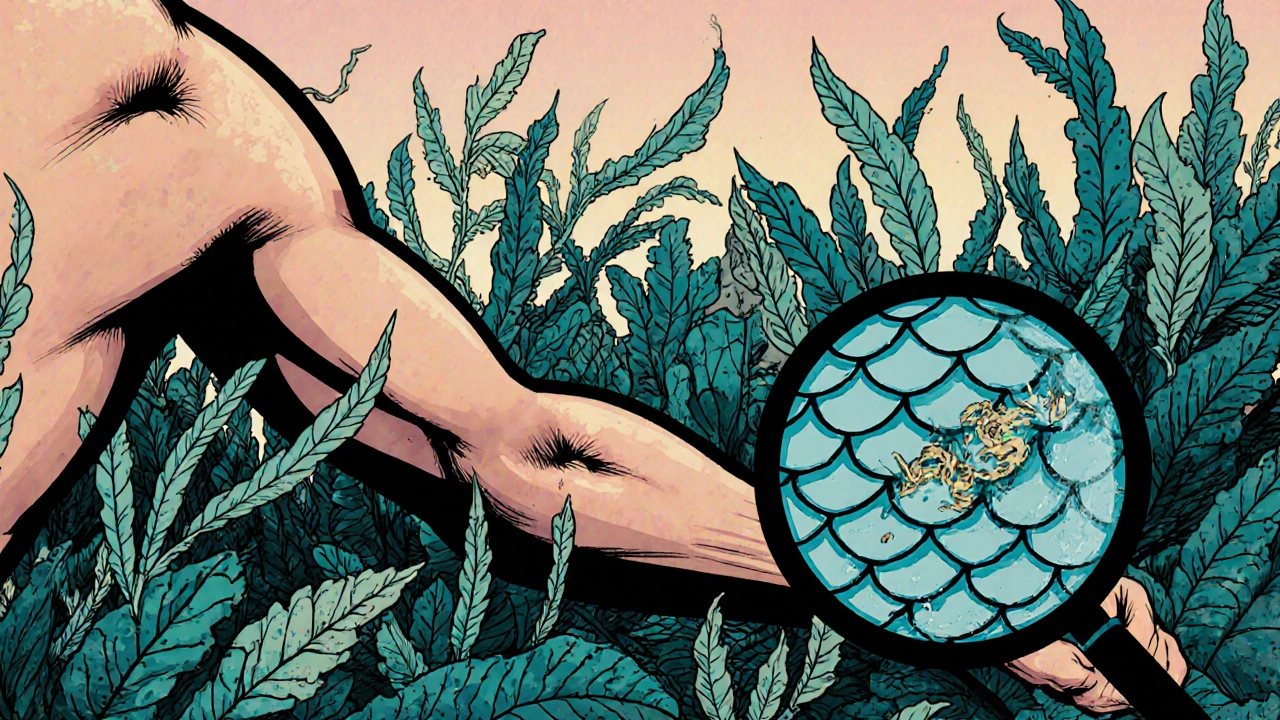
Skin is composed of layers, and the outermost layer - the stratum corneum - constantly renews itself. When that renewal process speeds up or the barrier gets compromised, the result is a build‑up of dead cells, known medically as hyperkeratosis. Think of it as a garden that’s over‑grown because the gardener (your body) either weeds too aggressively or stops watering altogether.
- Loss of natural oils → dryness and flaking.
- Accelerated cell turnover → thickened, plate‑like scales.
- Inflammation → redness, itching, and sometimes pain.
These basic mechanisms underlie almost every skin condition that presents with scales.
Top Conditions Behind Scaly Skin
Below are the most frequent diagnoses you’ll encounter. Each definition is marked up with schema.org microdata so search engines can surface the key facts quickly.
Psoriasis a chronic autoimmune disease that speeds up skin cell turnover, creating thick, silvery scales typically appears on elbows, knees, scalp, and lower back. The plaques are well‑defined, often itchy, and may crack, bleeding if not treated.
Eczema a group of inflammatory conditions that cause itchy, red, and sometimes scaly patches (also called atopic dermatitis) favours the creases of elbows and behind knees. The skin can become leathery over time.
Seborrheic Dermatitis a common rash that affects oily areas, producing greasy, yellow‑ish scales is most visible on the scalp, eyebrows, and around the nose.
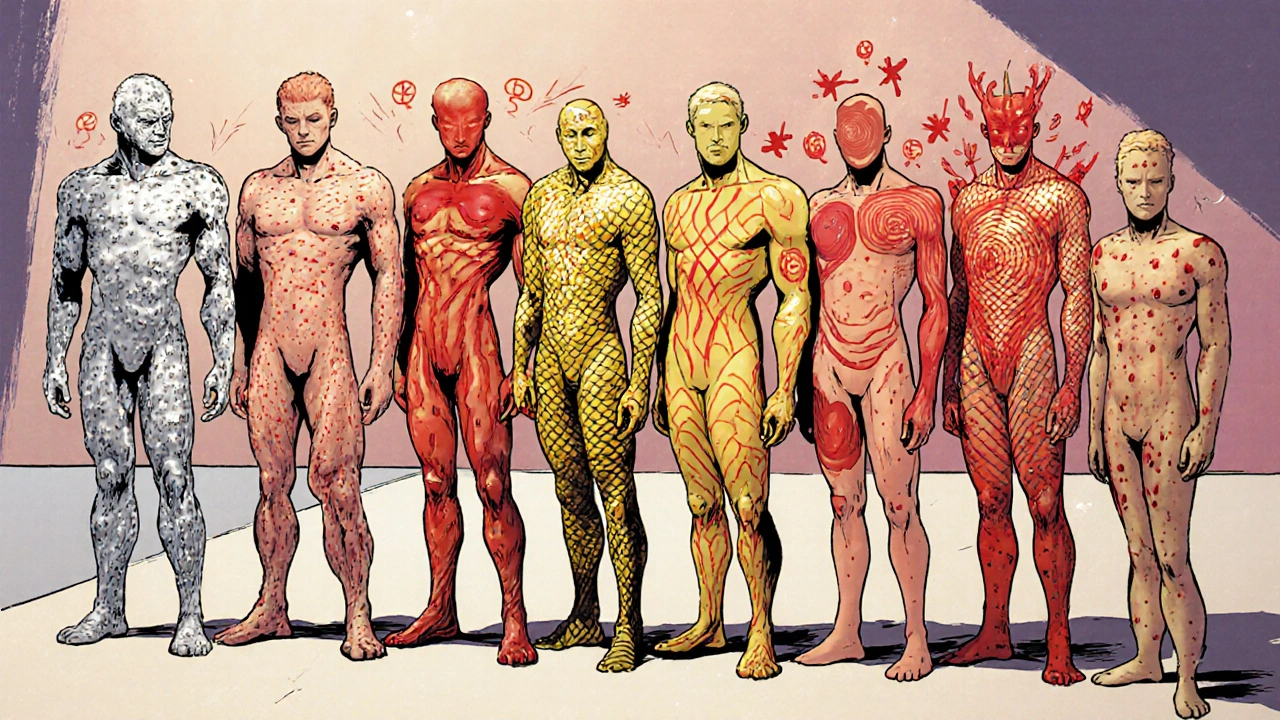
Ichthyosis a hereditary disorder where the skin retains a thick, fish‑scale appearance often shows up at birth or early childhood and can affect the entire body.
Fungal Infection skin‑invading fungi such as dermatophytes that cause ring‑shaped, scaly lesions (commonly called ringworm) spreads in warm, moist environments.
Contact Dermatitis an allergic or irritant reaction that leads to red, itchy, and sometimes scaly patches where a substance touched the skin can appear anywhere the offending material made contact.
Keratosis Pilaris a benign condition where keratin plugs hair follicles, leaving tiny, rough bumps that may feel scaly is most common on the upper arms and thighs.
How to Identify the Root Cause - A Practical Checklist
- Location: Are the scales confined to elbows/knees (psoriasis) or spread across the scalp (seborrheic dermatitis)?
- Scale Texture: Silvery and thick? Greasy and yellow? Dry and flaky?
- Itch Level: Mild irritation (keratosis pilaris) versus intense itch that interrupts sleep (eczema).
- Associated Redness or Swelling: Presence of well‑defined plaques points to psoriasis; diffuse redness suggests eczema or contact dermatitis.
- Trigger History: Recent new soap, detergent, or metal jewelry? Seasonal dryness? Family history of genetic skin disorders?
- Duration: Sudden outbreak (fungal infection) versus chronic years‑long presence (psoriasis, ichthyosis).
- Response to Over‑the‑Counter Products: Does a moisturiser help? Does a mild antifungal cream clear the rash?
Jot down your observations. When you eventually meet a dermatologist, this short log can cut down the number of tests needed.
When to Seek Professional Help
- Scales cover large areas or spread rapidly.
- Lesions bleed, crack, or develop pus.
- Over‑the‑counter remedies provide no relief after two weeks.
- You notice joint pain (possible psoriatic arthritis) or fever.
- Symptoms interfere with daily life or sleep.
Dermatologists can perform a quick skin scraping, a biopsy, or a simple Wood’s lamp exam to pinpoint the cause.
At‑Home Care Strategies that Actually Work
- Gentle, Fragrance‑Free Cleansers: Products labeled “soap‑free” help preserve the skin’s natural pH.
- Regular Moisturising: Apply a thick cream (e.g., petrolatum or ceramide‑rich lotion) within three minutes of a shower to lock in moisture.
- Targeted Topical Treatments:
- Low‑strength corticosteroid creams for flare‑ups (short‑term only).
- Salicylic acid or urea creams for thick plaques.
- Over‑the‑counter antifungal creams for ring‑shaped lesions.
- Lifestyle Tweaks: Keep humidity at 40‑60% in dry winter months, wear breathable fabrics, and avoid long, hot showers.
- Stress Management: Stress can trigger psoriasis and eczema flare‑ups; simple breathing exercises or short walks often help.
Consistency beats intensity. A few minutes each day of proper skin care can dramatically reduce scaling.

Comparison of the Most Common Scaly Skin Conditions
| Condition | Typical Appearance | Common Triggers | Usual Age of Onset | First‑Line Treatment |
|---|---|---|---|---|
| Psoriasis | Well‑defined, silvery‑white plaques | Stress, infection, injury (Koebner phenomenon) | Teens‑30s | Topical steroids, vitamin D analogues |
| Eczema (Atopic Dermatitis) | Red, itchy, often scaly patches | Allergens, dry air, sweating | Childhood, may persist | Moisturizers, low‑potency steroids |
| Seborrheic Dermatitis | Greasy, yellow‑ish scales on oily areas | Cold weather, stress, Malassezia yeast | Any age, common in infants (cradle cap) | Antifungal shampoos, mild steroids |
| Ichthyosis | Generalized dry, fish‑scale skin | Genetic mutation (no external trigger) | At birth or early childhood | Urea or lactic acid creams |
Quick Take‑aways
- Scaly skin is usually a sign of disrupted skin turnover or barrier loss.
- Location, texture, and itch level are the fastest clues to the underlying condition.
- Most mild cases improve with gentle cleansing, daily moisturisation, and targeted OTC creams.
- Seek a dermatologist if the rash spreads quickly, bleeds, or resists home treatment.
Frequently Asked Questions
Can I treat psoriasis at home?
Mild flare‑ups often respond to over‑the‑counter steroid creams and regular moisturisers. However, persistent or widespread plaques usually need prescription therapy from a dermatologist.
Why does my scalp get flaky while the rest of my skin stays smooth?
That pattern points to seborrheic dermatitis, which thrives on oily areas. An antifungal shampoo with ketoconazole or selenium sulfide often clears it within a few weeks.
Is dry skin the same as scaly overgrowth?
Dry skin (xerosis) can produce fine flakes, but true scaly overgrowth involves thicker, plate‑like buildup caused by accelerated cell turnover, as seen in psoriasis or eczema.
When should I worry about infection?
If the patches start oozing, develop pus, or become painful to touch, an infection may be setting in and you should see a doctor promptly.
Can stress really make my skin scaly?
Yes. Stress releases cortisol, which can flare psoriasis and eczema, making scales appear or worsen overnight.
Armed with the checklist and the comparison table, you can narrow down the likely cause of your scaly skin and take the right next steps-whether that means a new moisturiser, an OTC cream, or a dermatologist appointment.

The epidermis is organised in layers, so when the stratum corneum speeds up its turnover you’ll see that plate‑like build‑up first on areas with high friction. That’s why elbows and knees often betray psoriasis before anything else. If you notice a silvery sheen and the plaques feel firm, you’re probably looking at accelerated keratinocyte proliferation rather than simple dryness. On the other hand, greasy yellowish flakes point more toward seborrheic dermatitis, especially around the scalp and eyebrows. Keep an eye on any accompanying itch intensity – mild suggests keratosis pilaris, while a relentless scratch could hint at eczema.
I appreciate how the guide lays out a clear checklist; it makes the diagnostic process feel less intimidating. Noting the texture and distribution of scales can indeed narrow the differential quickly, which is especially helpful for those who dread endless doctor visits. The emphasis on gentle, fragrance‑free cleansers aligns with modern dermatological advice, and the reminder to moisturise within three minutes of a shower is a game‑changer for barrier repair. When you add the stress‑management tip, it acknowledges the mind‑skin connection that many overlook. Overall, this is a compassionate, thorough resource for anyone dealing with flaky skin.
Got the gist – moisturise early and check the scalp 😊
When you read about hyperkeratosis, it’s easy to think of it as just “more dead skin,” but the biology runs deeper. The epidermal turnover is regulated by a delicate balance of cytokines and growth factors; when that equilibrium tips, keratinocytes proliferate unchecked, leading to those thick, silvery plaques. Psoriasis, for example, is driven by Th17‑mediated inflammation, which explains why stress can flare it up overnight. Eczema, by contrast, often involves a compromised barrier and a Th2‑dominant response, making the skin red, itchy, and more prone to secondary infection. Seborrheic dermatitis thrives on Malassezia yeast, feeding on sebum, which is why oily areas become greasy and yellowish.
From a treatment standpoint, low‑strength corticosteroids are a double‑edged sword – they reduce inflammation but can thin the skin if overused, so limiting duration is crucial. Vitamin D analogues, such as calcipotriene, target the keratinocyte proliferation pathway without the atrophy risk. For fungal‑related scaling, an azole shampoo or topical terbinafine attacks the cell membrane of the organism, clearing the rings in a week or two.
Moisturising isn’t just about comfort; it restores the lipid matrix, preventing transepidermal water loss and reducing the itch‑scratch cycle. Ceramide‑rich creams mimic the natural skin lipids, while petrolatum creates an occlusive seal, trapping moisture. Applying within three minutes of a warm (not hot) shower maximises absorption because the skin’s pores are temporarily open.
Lifestyle adjustments also matter: a humidifier set to 45 % in winter keeps the stratum corneum hydrated, breathable fabrics reduce friction, and brief, lukewarm showers avoid stripping natural oils. Stress reduction techniques – guided breathing, short walks, or even a quick yoga session – can blunt the cortisol surge that aggravates both psoriasis and eczema.
If you see rapid spreading, bleeding, or pus formation, it’s a red flag that infection may have set in, and a dermatologist’s evaluation with a skin scraping or Wood’s lamp becomes necessary. In the meantime, avoiding harsh soaps, scrubbing aggressively, or picking at scales prevents secondary bacterial invasion.
Overall, the key is a systematic approach: identify the pattern, trial appropriate OTCs, and seek professional help when the rash resists or worsens. Consistency in skin care routines often outperforms occasional, intense treatments.
Great rundown! I’d add that staying consistent with the moisturiser, even on “good” days, can keep the barrier strong enough to fend off flare‑ups. It’s easy to slip when the skin looks clear, but the habit pays off long term.
I’ve battled dry elbows for years, and switching to a ceramide‑based lotion right after showering made a noticeable difference. I also kept a small travel‑size antifungal cream handy for any ring‑shaped patches that popped up after a beach trip.
From a pathophysiological perspective, the dysregulation of filaggrin expression plays a pivotal role in barrier compromise, especially in atopic eczema. Moreover, the hyperproliferative keratinocyte axis, mediated by IL‑17A and IL‑22, underlies the psoriatic phenotype. Targeted biologics that inhibit these cytokines have revolutionised therapeutic outcomes, reducing the hyperkeratotic scaling dramatically.
Ah, the age‑old battle of scales versus sanity – one might argue that our epidermal armor, when overzealous, becomes a tapestry of medieval parchment, demanding the counsel of modern alchemists armed with corticosteroids and vitamin D analogues. Yet, truly, the art lies in discerning whether one’s skin is merely reciting a chorus of dryness or staging a full‑blown theatrical rendition of auto‑immune drama.
Interesting take, but I still think a good old soap‑free wash does the trick most days 😂
Your checklist is spot on – especially the part about tracking response to OTC products. It saves a lot of time before jumping to a dermatologist.
The article oversimplifies the diagnostic process; many clinicians rely on dermoscopy and histopathology to differentiate between conditions that appear clinically similar.