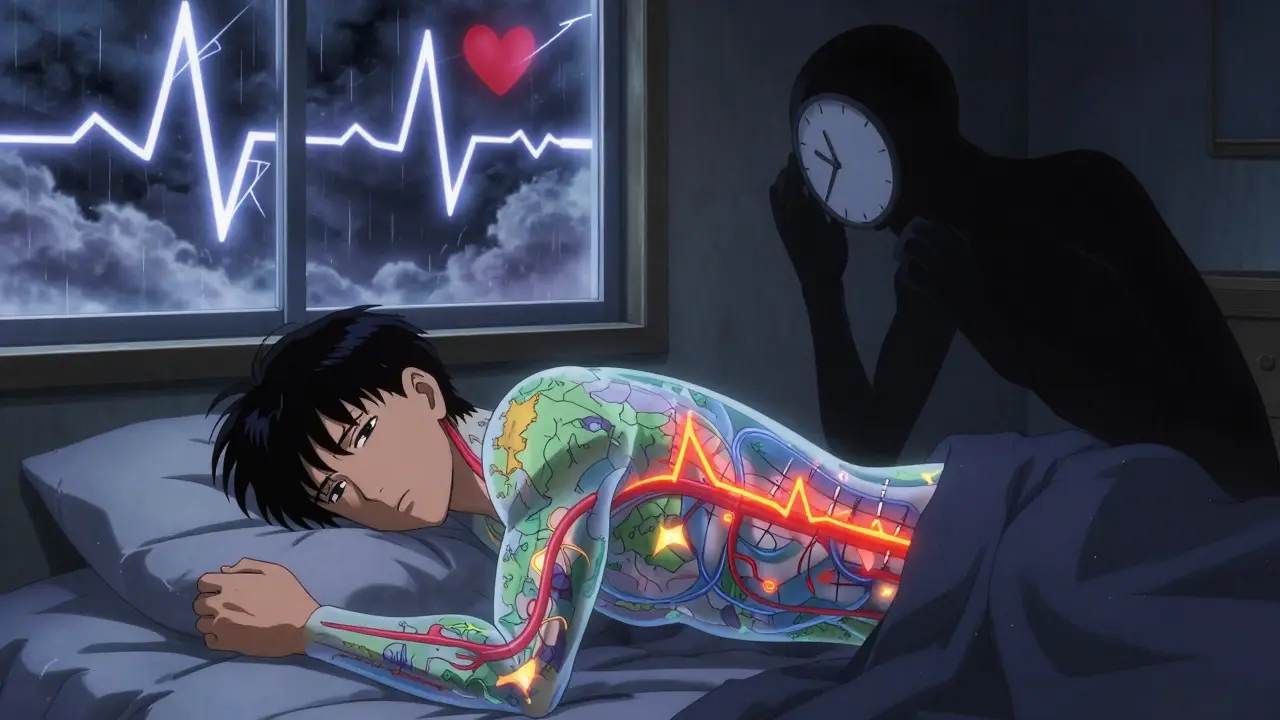
When you stop breathing for 10 seconds-repeatedly-while you sleep, your body doesn’t just wake you up. It triggers a cascade of stress responses that can damage your heart, raise your blood pressure, and set the stage for a heart attack or stroke. This isn’t just snoring. This is sleep apnea, and it’s silently increasing your risk of life-threatening heart problems.
What Exactly Is Sleep Apnea?
Sleep apnea means your breathing stops and starts during sleep. The most common type, obstructive sleep apnea (OSA), happens when the muscles in your throat relax too much and block your airway. You might not even know it’s happening. You don’t wake up fully-you just shift into a lighter stage of sleep so your body can restart breathing. This cycle can repeat 30 times or more per hour, every night.Eighty to ninety percent of sleep apnea cases are obstructive. The rest are central, where your brain fails to send the right signals to breathe. But OSA is the real public health crisis. About 1 billion people worldwide have it, including 40 million in the U.S. alone. And here’s the scary part: 80% of people with moderate to severe sleep apnea don’t even know they have it.
Obesity is the biggest driver. The American Heart Association says 70% of OSA cases are directly tied to excess weight. Fat around the neck narrows the airway. Fat in the abdomen pulls down on the diaphragm. Both make breathing harder during sleep.
How Sleep Apnea Kills Your Heart
Every time your airway collapses, your oxygen levels drop. Your body panics. Your heart rate spikes. Your blood pressure surges. Your stress hormones-epinephrine and norepinephrine-skyrocket, sometimes two to four times higher than normal during sleep. This isn’t a one-time event. It happens dozens of times a night, every night.Over time, this constant stress rewires your cardiovascular system:
- High blood pressure: Up to 80% of people with resistant hypertension-blood pressure that won’t drop even after taking three different medications-have undiagnosed sleep apnea. OSA patients are two to three times more likely to develop high blood pressure within just four to five years.
- Non-dipping blood pressure: Normally, your blood pressure drops 10% or more at night. In 70-80% of people with OSA, it doesn’t drop at all. Some even rise. This pattern is linked to a much higher risk of heart attack and stroke.
- Inflammation and damage: Chronic low oxygen triggers inflammation. C-reactive protein, a marker of body-wide inflammation, is 35-50% higher in OSA patients. Blood vessels lose their ability to relax properly. Flow-mediated dilation-a measure of artery health-drops by 25-40%. Oxidative stress markers like malondialdehyde rise two to three times above normal.
These changes don’t just make you feel tired. They directly damage your heart and arteries.
Heart Disease, Stroke, and the Silent Connection
If you have moderate to severe sleep apnea (Apnea-Hypopnea Index ≥15), your risk of heart disease jumps:- 30% higher risk of coronary artery disease
- 140% higher risk of heart failure
- 1.3 times more likely to have a heart attack
- 1.6 times more likely to die from a coronary event
And it’s not just about the heart. Stroke risk is even more alarming. OSA increases your chance of having your first stroke by 2.5 times. If you’ve already had a stroke, your risk of another one jumps 3.2 times. The worse your oxygen drops at night, the deadlier it gets-people with oxygen saturation below 90% for more than 12% of sleep time have 4.3 times higher stroke mortality.
There’s also a strange timing pattern. Nearly 27% of heart attacks in people with sleep apnea happen between midnight and 6 a.m.-a time when blood pressure normally drops. In people without OSA, that number is only 16.5%. This suggests sleep apnea isn’t just a risk factor-it’s an active trigger.

Heart Failure and Arrhythmias: A Dangerous Loop
Heart failure and sleep apnea often go hand in hand. About 40-60% of people with heart failure also have sleep apnea. But it’s not just a coincidence. OSA makes heart failure worse by forcing the heart to work harder against rising pressure in the chest. It also causes irregular heart rhythms.Atrial fibrillation (AFib)-the most common dangerous heart rhythm-is twice as common in people with OSA. In one study, 49% of people with paroxysmal AFib had sleep apnea, compared to just 21% of those without it. And if you’re getting catheter ablation for AFib, your success rate drops by 30% if your sleep apnea is untreated.
Even cardiac resynchronization therapy (CRT), a device used for heart failure, works less effectively in patients with untreated OSA. Their response rate drops by 15%.
Why Younger People Are at Greater Risk
Most people assume sleep apnea is an older adult problem. But recent data shows it’s hitting younger people harder than we thought. A 2024 study of nearly 10,000 adults found that people aged 20-40 with OSA symptoms had a 45% higher chance of high blood pressure, 33% higher chance of diabetes, and 25% higher chance of metabolic syndrome compared to peers without symptoms.In people over 41, the increase was only 10-12%. That means sleep apnea isn’t just aging-it’s accelerating disease. For younger adults, it’s not a slow burn. It’s a fast track to heart problems.
CPAP Isn’t a Magic Bullet-But It Still Saves Lives
The go-to treatment for OSA is CPAP-a machine that blows air through a mask to keep your airway open. It’s effective, but not perfect.CPAP only lowers blood pressure by 2-3 mmHg on average. That’s not enough to make a big difference for most people with high blood pressure. But here’s what it does do:
- Reduces stroke recurrence by 37%
- Improves outcomes in heart failure patients with central sleep apnea
- Increases success rates for AFib ablation
- Improves response to heart failure devices
So while CPAP might not cure your high blood pressure, it stops the damage from getting worse. And that matters.
But here’s the catch: only 46% of people who get a CPAP machine use it enough-4 hours a night, 70% of nights. Without consistent use, the benefits vanish. Many quit because the mask is uncomfortable, the machine is noisy, or they don’t feel better right away.
What Cardiologists Are Starting to Do
The American Heart Association now says: Screen for sleep apnea in every patient with high blood pressure, atrial fibrillation, heart failure, stroke, or coronary artery disease. Especially if their condition isn’t responding to treatment.Simple tools like the STOP-Bang questionnaire-asking about snoring, tiredness, high blood pressure, BMI, age, neck size, and gender-can catch 84% of moderate to severe cases. It takes less than a minute. Yet most heart clinics don’t use it.
Cardiologists are starting to push for better collaboration with sleep specialists. No more silos. If you have heart disease and you’re tired all day, or your partner says you stop breathing at night, it’s not just “getting old.” It’s a warning sign.
What You Should Do Now
If you have any of these, get checked for sleep apnea:- High blood pressure that won’t go down
- Irregular heartbeat (especially atrial fibrillation)
- Heart failure
- Had a stroke or mini-stroke
- Snore loudly, wake up gasping, or feel exhausted despite sleeping 8 hours
- Are overweight and under 40
You don’t need a full overnight sleep study right away. Home sleep tests are 85-90% accurate for moderate to severe OSA. If you’re at risk, start there.
Don’t wait for a heart attack. Don’t assume your fatigue is just stress. Sleep apnea isn’t a sleep problem-it’s a heart problem in disguise.
Can sleep apnea cause high blood pressure even if I’m not overweight?
Yes. While obesity is the biggest risk factor, sleep apnea can happen in thin people too. Structural issues like a narrow airway, large tonsils, or jaw position can cause it. Even without extra weight, repeated drops in oxygen during sleep trigger stress hormones and raise blood pressure. If you have unexplained high blood pressure, sleep apnea should still be ruled out.
Does treating sleep apnea lower the risk of a heart attack?
Treating sleep apnea doesn’t guarantee you won’t have a heart attack, but it significantly reduces your risk. Studies show that consistent CPAP use lowers the chance of fatal heart events by up to 40% over time. It also reduces the number of heart attacks that happen at night, which are more deadly. The key is consistent use-skipping nights means the protection fades.
Why does my blood pressure stay high even after taking three medications?
If your blood pressure remains high despite three different drugs, you may have resistant hypertension-and sleep apnea is the most common hidden cause. Up to 80% of people with resistant hypertension have undiagnosed OSA. Treating the sleep apnea often brings blood pressure down significantly, sometimes allowing you to reduce or eliminate medications.
Can I use a mouthpiece instead of CPAP for sleep apnea?
Oral appliances can work for mild to moderate sleep apnea, especially if you can’t tolerate CPAP. They reposition your jaw to keep the airway open. But for severe OSA or if you have heart disease, CPAP is still the gold standard. Mouthpieces don’t reduce cardiovascular risk as reliably. Always talk to a sleep specialist before switching treatments.
Is sleep apnea only a problem for older adults?
No. While it’s more common with age, young adults (20-40) with sleep apnea face a much higher relative risk of high blood pressure, diabetes, and metabolic syndrome than older adults. Sleep apnea may be accelerating cardiovascular disease in younger people, making early screening critical-even if you feel fine.

Wow. I never realized how much my snoring was actually my heart screaming for help. I thought it was just being tired from work, but now I get why I wake up like I ran a marathon. I’m getting tested this week. Thanks for laying it out like this - it’s scary but also empowering.
Same here I used to think sleep apnea was just for old guys who snore like chainsaws now I see it’s a silent killer and I’m 34 and overweight and tired all the time
Let’s be real here. The medical industrial complex has turned sleep apnea into a cash cow. CPAP machines cost $800 and are barely effective. The real solution is weight loss and positional therapy. But no one wants to hear that because it requires effort. Instead we sell you a mask and call it a day. Meanwhile, the real epidemic is processed food and sedentary lifestyles. The system doesn’t want you to fix the root cause - it wants you to buy the product.
Look at the stats: 80% of OSA cases tied to obesity. So why are we spending billions on machines instead of subsidizing vegetables and banning soda in hospitals? This isn’t medicine - it’s corporate triage disguised as care.
And don’t get me started on the ‘STOP-Bang’ questionnaire. It’s a band-aid on a hemorrhage. You’re not screening for sleep apnea - you’re screening for who can afford to be screened. Meanwhile, the guy working two jobs and sleeping in his car? He’s just gonna keep dying quietly.
The data is clear. The solutions are obvious. The will to act? Nonexistent. Welcome to American healthcare: expensive, reactive, and fundamentally dishonest.
I’ve been using a mouthpiece for 6 months and honestly it’s been life-changing. I used to wake up with headaches every day. Now I feel like I actually slept. I know CPAP is the gold standard but if you can’t stand it, don’t give up - there are other options. Talk to your sleep doc, don’t just accept the first thing they hand you.
My husband snores so loud the dog sleeps in the other room and he says he’s fine but I know he’s not - he’s always irritable and he’s got high BP and he refuses to get tested I’m so tired of watching him slowly kill himself
People are so lazy. You think a machine is gonna fix your 300-pound body? Wake up. If you’re not willing to lose weight, stop pretending you care about your heart. CPAP is just a crutch for people who refuse to change. You want to live? Eat less. Move more. Stop blaming your airway for your poor life choices.
I’m a cardiologist and I’ve seen this firsthand. I had a 38-year-old patient with no family history of heart disease - had a heart attack at 35. Turns out he had severe OSA. No obesity. Just a narrow airway. He’s on CPAP now. His BP dropped 20 points. His AFib stopped. He’s back to coaching his kid’s soccer team. This isn’t theoretical - it’s life or death. Get tested. No excuses.
Why are we even talking about this? In Russia, they just tell you to sleep on your side and drink black tea. No machines. No masks. No $2000 bills. We don’t overmedicalize everything. America turns a yawn into a crisis and sells you a $1000 box to fix it. Meanwhile, the rest of the world just… lives. Maybe the problem isn’t your airway - it’s your mindset.
Oh so now sleep apnea is a heart disease? Next they’ll say coughing causes lung cancer. You know what causes heart disease? Sugar. Stress. Corporate greed. Not your nose. Not your tongue. Not your stupid mask. You think your body’s failing? Nah. The system is. They sell you CPAP because it’s profitable. They don’t sell you broccoli because it doesn’t have a patent. Wake up. You’re being played.
Just got my home sleep test results - severe OSA 😭 I cried for 20 minutes. But then I remembered - I can fix this. I’m ordering a CPAP tomorrow. And I’m starting yoga. And I’m cutting out soda. I got this. 💪❤️
my doc said i have it but i dont feel tired so maybe its not real
Isn’t it strange how we treat the body like a machine you break, you fix - but we forget it’s alive? Sleep apnea isn’t a glitch in the system. It’s a message. Your body is screaming for stillness. For rhythm. For less sugar. Less stress. Less screens. The CPAP is just a bandage on a wound that’s been caused by a culture that values productivity over presence. Maybe the real treatment isn’t air pressure - it’s surrender. To rest. To silence. To sleep.