Calcium Deficiency – What It Means for Your Health
When talking about calcium deficiency, a condition where the body lacks enough calcium for normal bone and muscle function. Also known as low calcium, it can sneak up on you through poor diet, gut issues, or hormone problems. Osteoporosis, a disease marked by fragile, porous bones often shows up when calcium deficiency goes unchecked. Vitamin D deficiency, insufficient vitamin D that hampers calcium absorption is another common partner, while parathyroid hormone imbalance, disruption in the hormone that regulates calcium levels can either cause or result from low calcium. Understanding these links helps you spot the problem early and take action.
How Calcium, Vitamin D, and Hormones Work Together
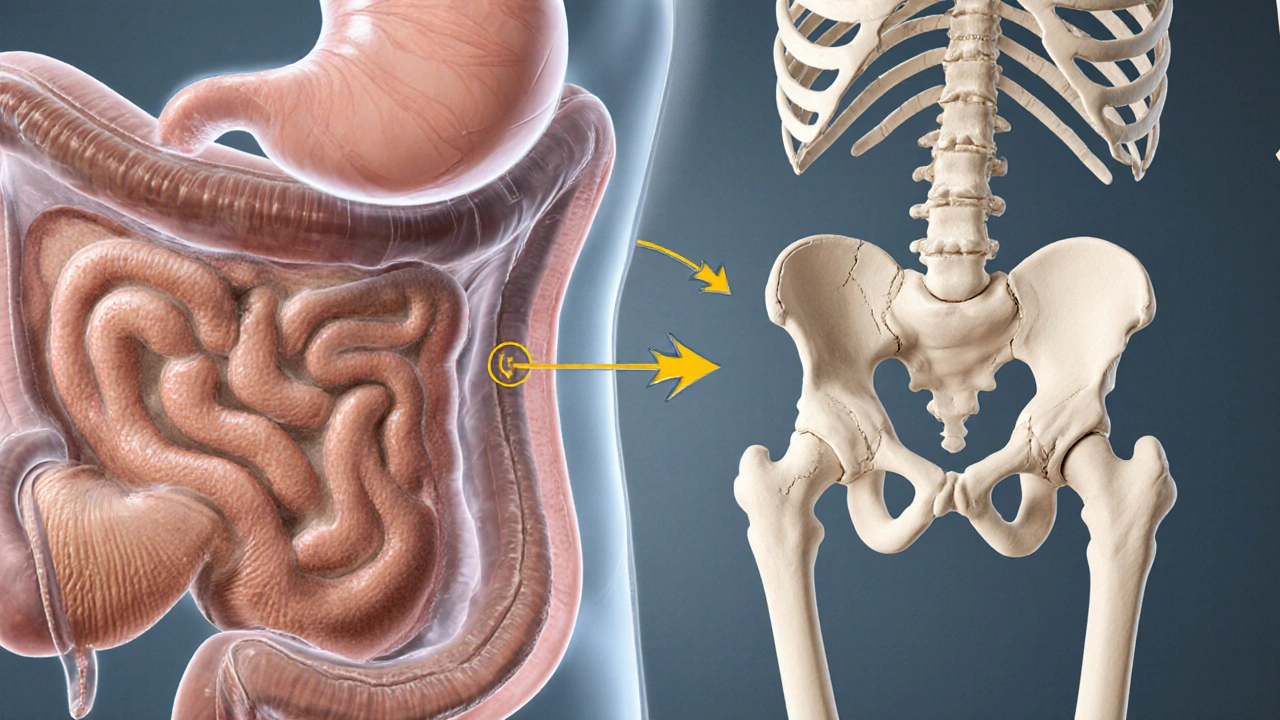
Think of calcium as the building block, vitamin D as the delivery truck, and parathyroid hormone as the traffic controller. When vitamin D levels are adequate, the gut pulls calcium from food into the bloodstream efficiently. If vitamin D drops, that delivery slows, and the body taps the parathyroid hormone to pull calcium from bones, which over time weakens them. This chain reaction explains why chronic calcium deficiency often leads to osteoporosis. A simple semantic triple here: Calcium deficiency reduces bone density; Vitamin D deficiency reduces calcium absorption; Parathyroid hormone imbalance increases bone resorption.
Diet matters too. Most adults need about 1,000 mg of calcium daily, but many fall short because they skip dairy, leafy greens, or fortified foods. Even when intake looks good on paper, gut health can sabotage absorption. Conditions like atrophic gastroenteritis or chronic use of acid‑reducer drugs (think Prilosec) lower stomach acidity, which is needed to dissolve calcium salts. When the gut isn’t doing its job, the calcium you eat never makes it to the bloodstream, and the hormone loop kicks in.
Age and lifestyle add more layers. Post‑menopausal women often see a spike in parathyroid hormone activity, draining calcium from bones faster than it can be replaced. Athletes on high‑protein or low‑carb diets may also experience increased calcium loss through urine. And let’s not forget that obesity can hide a calcium shortage; excess weight puts extra strain on bones, accelerating the need for calcium while inflammatory signals interfere with vitamin D activation.
So what can you do right now? Start with a quick calcium audit: tally up dairy, fortified plant milks, tofu, sardines, and leafy greens you eat in a typical day. Pair those foods with a reliable source of vitamin D—sun exposure, oily fish, or a supplement that provides at least 800 IU daily. If you’re on long‑term acid‑reducer therapy, talk to your doctor about a calcium citrate supplement, which absorbs better without strong stomach acid. Finally, get your parathyroid hormone levels checked if you have unexplained bone pain or frequent fractures; a simple blood test can reveal whether the hormone is over‑working.
The articles below dive deeper into each piece of the puzzle. You’ll find guides on how specific medications affect calcium balance, what supplements really work, and practical steps to protect your bones whether you’re an athlete, a senior, or anyone in between. Keep reading to get the details you need to turn this knowledge into healthier habits.