INR Elevation Risk Calculator
INR Elevation Calculator
This tool estimates how trimethoprim-sulfamethoxazole may affect your INR while taking warfarin. Based on clinical studies, this antibiotic typically increases INR by 1.8 points on average.
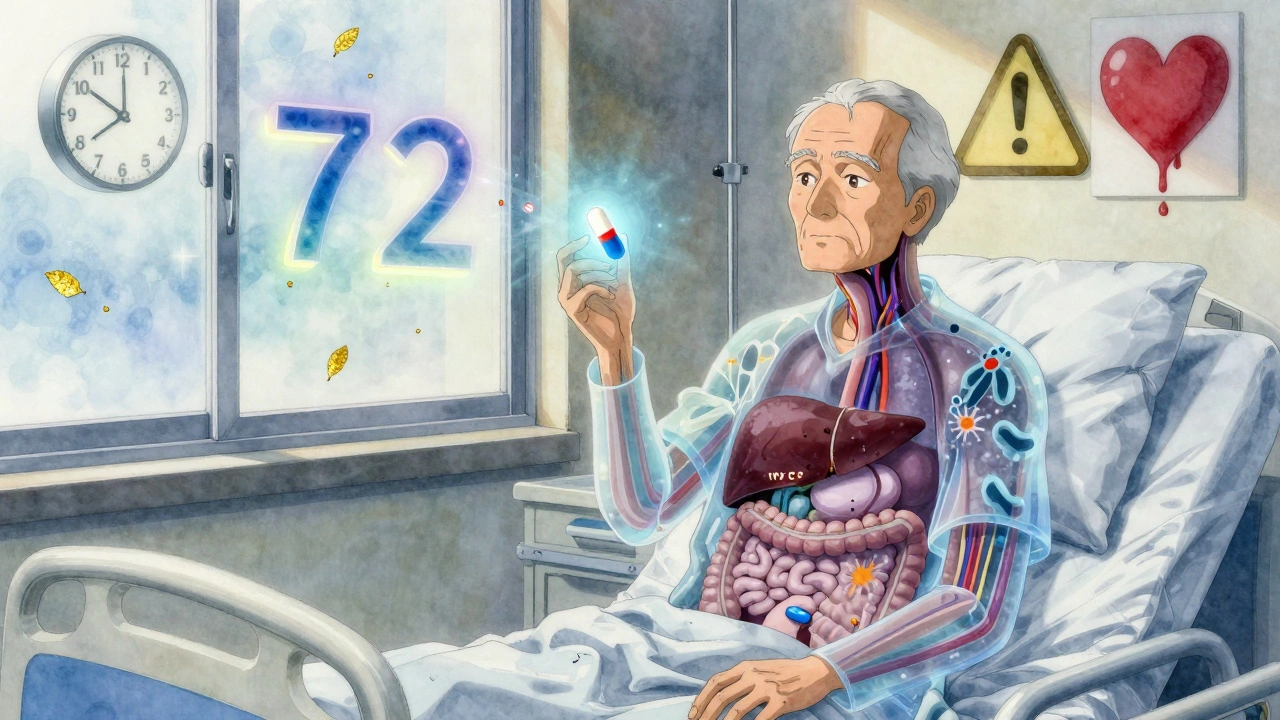
When you're on warfarin, even a simple antibiotic can turn dangerous. Trimethoprim-sulfamethoxazole - commonly sold as Bactrim or Septra - is one of the most common antibiotics prescribed for urinary tract infections, sinus infections, and bronchitis. But if you're taking warfarin for atrial fibrillation, a mechanical heart valve, or deep vein thrombosis, mixing these two can send your INR through the roof. And that’s not just a lab number. It’s a warning sign your blood is thinning too much, putting you at risk of internal bleeding, stroke, or even death.
Why This Interaction Happens
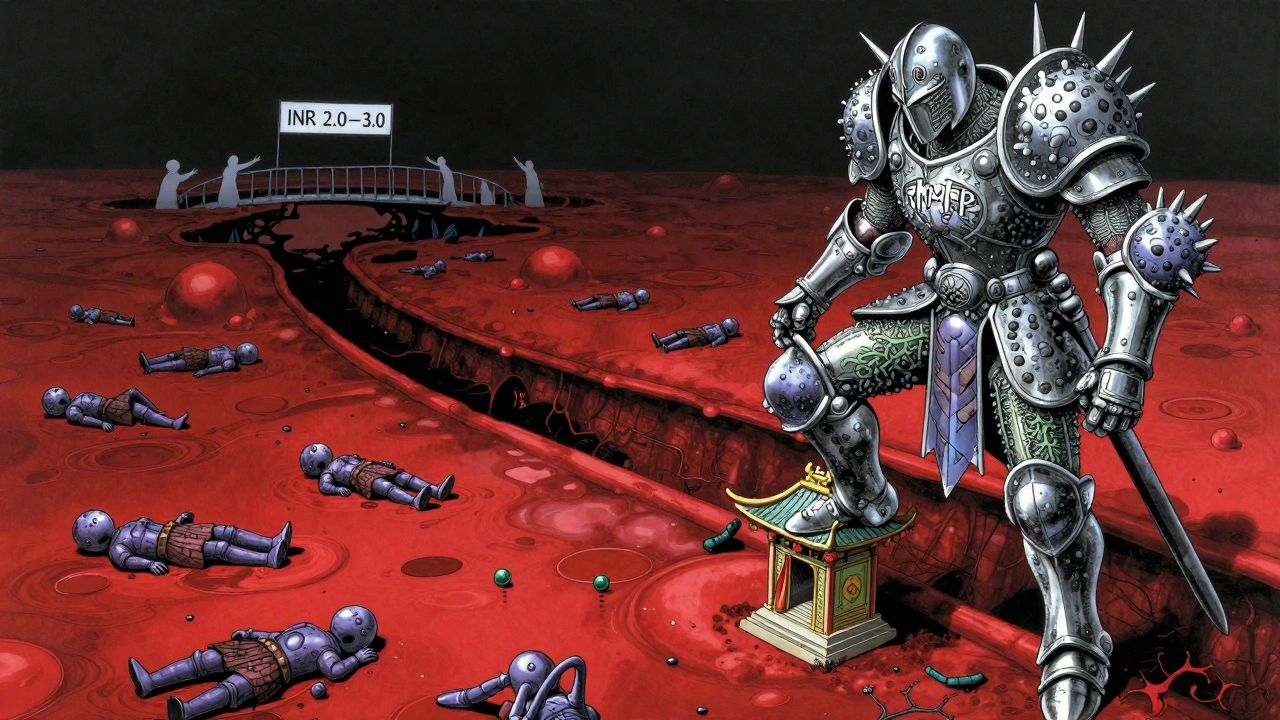
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a delicate balance. Too little, and you clot too easily. Too much, and you bleed uncontrollably. The drug is 97-99% bound to proteins in your blood, leaving almost no room for other drugs to sneak in. That’s where trimethoprim-sulfamethoxazole comes in.This antibiotic doesn’t just fight bacteria - it interferes with warfarin in three ways. First, sulfamethoxazole pushes warfarin off its protein binding sites, flooding your bloodstream with free, active warfarin. Second, trimethoprim blocks the CYP2C9 enzyme, the main system your liver uses to break down the more powerful S-warfarin molecule. This slows warfarin clearance by 20-30%. Third, the antibiotic wipes out gut bacteria that make vitamin K. Less vitamin K means warfarin works even harder.
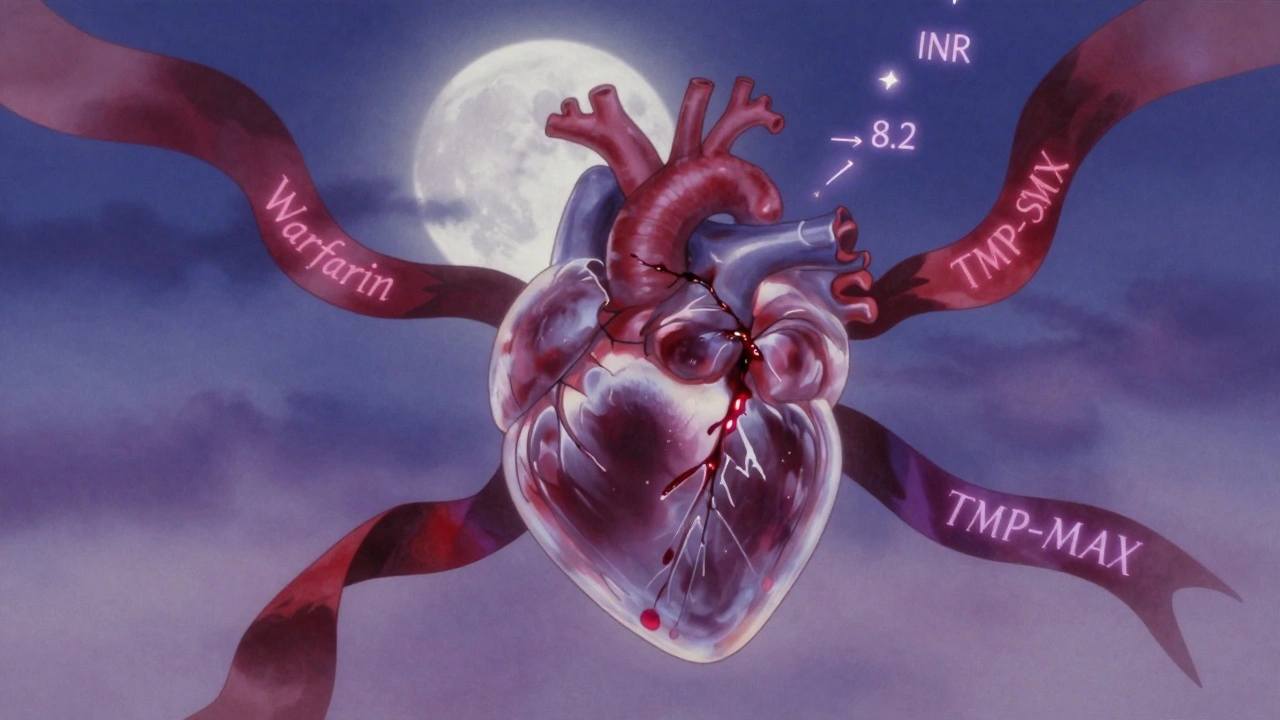
These effects don’t show up overnight. INR typically spikes within 36 to 72 hours after starting the antibiotic. That’s why many patients don’t realize the danger until they’re already bleeding - a nosebleed that won’t stop, bruising without injury, or worse, blood in their urine or stool.
How Much Does INR Really Rise?
Not all antibiotics are equal when it comes to warfarin. A 2023 study tracking over 70,000 patients found that TMP-SMX increased INR by an average of 1.8 points. That’s not a small jump. For someone with a stable INR of 2.5, that’s a leap to 4.3 - well above the safe range of 2.0-3.0 for most conditions.Compare that to amoxicillin, which only raised INR by 0.4 points on average. Ciprofloxacin? About 0.9. TMP-SMX isn’t just a mild interaction - it’s one of the strongest. And it’s not random. The FDA’s adverse event database recorded 1,842 cases of INR elevation linked to TMP-SMX over five years. Nearly half led to hospitalization. Nearly 4% ended in fatal bleeding.
Some people are more at risk. Patients over 75, those with heart failure, liver disease, or poor nutrition saw INR increases of 2.5 points or more. Men were 9% more likely than women to experience dangerous spikes. Why? Not fully clear - but it may relate to body weight, liver enzyme activity, or even differences in gut flora.
Real Cases, Real Consequences
A 78-year-old man with a mechanical aortic valve was prescribed Bactrim for a chest infection. His INR had been steady at 2.8 for months. Three days later, he collapsed with internal bleeding. His INR was 8.2. He needed vitamin K, fresh frozen plasma, and spent a week in the ICU. His story isn’t rare.On patient forums, nurses and caregivers share similar experiences: INR jumping from 2.5 to 6.0 after just two days of Bactrim. One pharmacist on Reddit said she’s seen patients take it without issue - but that’s the exception. Variability doesn’t mean safety. It means unpredictability. And with warfarin, unpredictability kills.
The American Heart Association, the Institute for Safe Medication Practices, and the American College of Chest Physicians all list this interaction as high-risk. Yet, a 2022 study in JAMA Internal Medicine found nearly 1 in 5 warfarin patients still got a potentially dangerous antibiotic within 30 days. TMP-SMX made up almost 30% of those prescriptions.
What Should You Do?
If you’re on warfarin and your doctor suggests TMP-SMX, ask: Is there a safer alternative?For urinary tract infections, nitrofurantoin or fosfomycin are often better choices. For sinus infections, amoxicillin or doxycycline usually don’t interfere. For pneumonia, azithromycin or levofloxacin (with caution) might be options. Always check with your pharmacist or anticoagulation clinic before starting any new medication.
If TMP-SMX is truly necessary - say, for a severe infection with no alternatives - here’s what to do:
- Check your INR before starting the antibiotic.
- Reduce your warfarin dose by 20-30% as a precaution - especially if you’re over 70 or have liver issues.
- Test your INR again within 48 hours. Then every 2-3 days while on the antibiotic.
- Watch for signs of bleeding: unusual bruising, pink or red urine, black stools, headaches, dizziness, or vomiting blood.
If your INR climbs to 4.0-5.0 and you’re not bleeding, skip 1-2 warfarin doses and restart at a lower dose. If your INR is above 5.0 with minor bleeding, take 1-2.5 mg of oral vitamin K. If you’re bleeding heavily or your INR is above 10, you need emergency treatment: IV vitamin K and a clotting factor concentrate like 4-factor prothrombin complex.
Education Saves Lives
Many patients don’t know this interaction exists. The National Blood Clot Alliance found that people who got specific counseling about antibiotic-warfarin risks had 37% fewer emergency visits for bleeding. That’s not a small difference. That’s life or death.Don’t assume your doctor will always warn you. Pharmacists are your second line of defense. Ask: “Does this antibiotic interact with my blood thinner?” Write it down. Bring a list of all your meds - including supplements - to every appointment.
The Bigger Picture
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban have replaced warfarin for many people. They’re easier to use, don’t need regular blood tests, and have fewer food and drug interactions. But 2.6 million Americans still take warfarin. Why? Because DOACs aren’t right for everyone. Patients with mechanical heart valves, severe kidney disease, or certain clotting disorders still need warfarin.And until those patients are gone - and that’s not happening soon - this interaction will remain a silent killer in clinics and hospitals. The NIH is funding a $2.4 million study to predict who’s most at risk, using genetics and clinical data. But until then, the rules are simple: avoid TMP-SMX if you can. If you can’t, monitor closely. And never ignore a rising INR.
When to Call for Help
If you’re on warfarin and start TMP-SMX, call your doctor or anticoagulation clinic immediately if you notice:- Bleeding that won’t stop after 10 minutes
- Red or brown urine
- Black, tarry stools
- Severe headache or vision changes
- Unexplained swelling or pain
- INR above 5.0
Don’t wait. Don’t assume it’s just a “bad day.” This interaction moves fast. Your INR can go from safe to life-threatening in under 72 hours.

I got prescribed Bactrim last year for a UTI and didn't think twice. My INR was fine until day three - then I started bruising like a cartoon. Didn't even know it was the antibiotic until my pharmacist called me out of nowhere. Scary stuff.
Don't assume your doctor knows every interaction. Always ask.
Of course the FDA has a database of 1,842 cases - because Americans can't take responsibility for their own health anymore. You take a blood thinner? Then you learn what it does. Stop outsourcing your brain to Big Pharma and their fear-mongering pamphlets.
Meanwhile, in Japan, people take warfarin with soy sauce and never blink. Maybe we should stop treating ourselves like fragile porcelain.
This is exactly why we need better patient education - not just in clinics, but in schools, pharmacies, even social media. I'm a nurse and I still see patients on warfarin who think "antibiotic" means "safe."
It’s not about fear. It’s about awareness. And awareness saves lives. If we all took five minutes to learn one interaction, we could prevent so much suffering.
Thank you for writing this. It’s clear, thorough, and human.
I had a friend who took Bactrim while on warfarin and woke up with a headache so bad she thought she was having a stroke. Turns out her INR was 7.1. She spent three days in the hospital getting vitamin K IVs. Her dog sat outside her room the whole time. She still talks about it like it was a horror movie.
It’s wild how something so common - like a sinus infection - can turn into a nightmare if you’re not paying attention. I now keep a little card in my wallet that says "NO BACTRIM" next to my warfarin dose. Small thing. Big difference.
Did you know the CDC secretly tracks all INR spikes and hides them from the public? They don’t want you to know how many people die from "routine" antibiotics. And Bactrim? It’s not even the worst one. They’ve been pushing it for decades because it’s cheap and pharma makes bank.
They don’t care if you bleed out - they care about your insurance copay. Look up the 2019 whistleblower report. It’s all there. They’re killing people to keep profits high.
The assertion that TMP-SMX constitutes a "high-risk" interaction is empirically supported by multiple authoritative bodies. However, the implication that clinicians routinely neglect this interaction is misleading. Standard electronic health record systems now flag this combination with tier-one alerts. The issue lies not in clinical ignorance, but in patient non-adherence to monitoring protocols.
Furthermore, the suggestion to reduce warfarin dose preemptively lacks robust evidence in the current literature. Such practice may induce thrombotic events, which are equally lethal.
Let me tell you something about Western medicine - it’s built on fear, not wisdom. You take warfarin? You become a lab rat. You need an antibiotic? You’re told to panic. But in India, we’ve been using natural remedies for centuries - turmeric, neem, garlic - and we don’t need to check our INR every three days.
Why do you let corporations control your body? Why do you trust a machine over your own intuition? The real problem isn’t Bactrim. It’s your dependence on systems that profit from your vulnerability.
Wake up.
okay so i just found out my doc prescribed me bactrim last month and i was on warfarin and i didnt even know this was a thing??
now im paranoid af. did i bleed internally?? am i gonna die??
my INR was 2.7 last week... i think i’m fine?? but now i can’t sleep. help.
Thanks for posting this. I’ve been on warfarin for 12 years and never knew about this until now.
My pharmacist flagged it when I picked up my script - I didn’t even think to ask. I’m so glad I listened.
Small things matter. I’m printing this out and putting it on my fridge.
❤️
While the pharmacokinetic mechanisms elucidated are scientifically accurate, it is imperative to emphasize that individual variability in CYP2C9 and VKORC1 genotypes significantly modulates the magnitude of INR elevation. Genetic testing prior to initiating concomitant therapy may offer a personalized risk stratification approach, thereby mitigating adverse outcomes.
Furthermore, the reliance on population-based INR thresholds may not adequately reflect the therapeutic needs of patients with mechanical heart valves, who often require higher INR targets. Clinical judgment remains paramount.
Let’s not sugarcoat this: TMP-SMX is a pharmacological landmine for anticoagulated patients. The 1.8-point INR spike isn’t a "risk" - it’s a guaranteed pharmacodynamic cascade. And the fact that 1 in 5 patients still get this combo? That’s not negligence. That’s systemic malpractice.
Healthcare systems are designed to optimize throughput, not safety. Your INR isn’t a number - it’s a death sentence waiting to be triggered. And they still prescribe it like it’s Advil.
There’s a quiet heroism in patients who ask questions. I’ve seen people who’ve survived because they said, "Wait, what’s this for?" - and then checked with their pharmacist.
This isn’t about fear. It’s about power. You have the right to understand what’s going into your body. Don’t let anyone make you feel silly for asking.
And if you’re on warfarin? Keep a little notebook. Write down every med, every dose, every INR. It’s not paranoia - it’s self-care.
You’re not a burden. You’re a partner in your own healing.