Atrophic Gastroenteritis Symptom Checker
This tool helps identify possible early signs of Atrophic Gastroenteritis. Answer the questions below to get a personalized risk assessment.
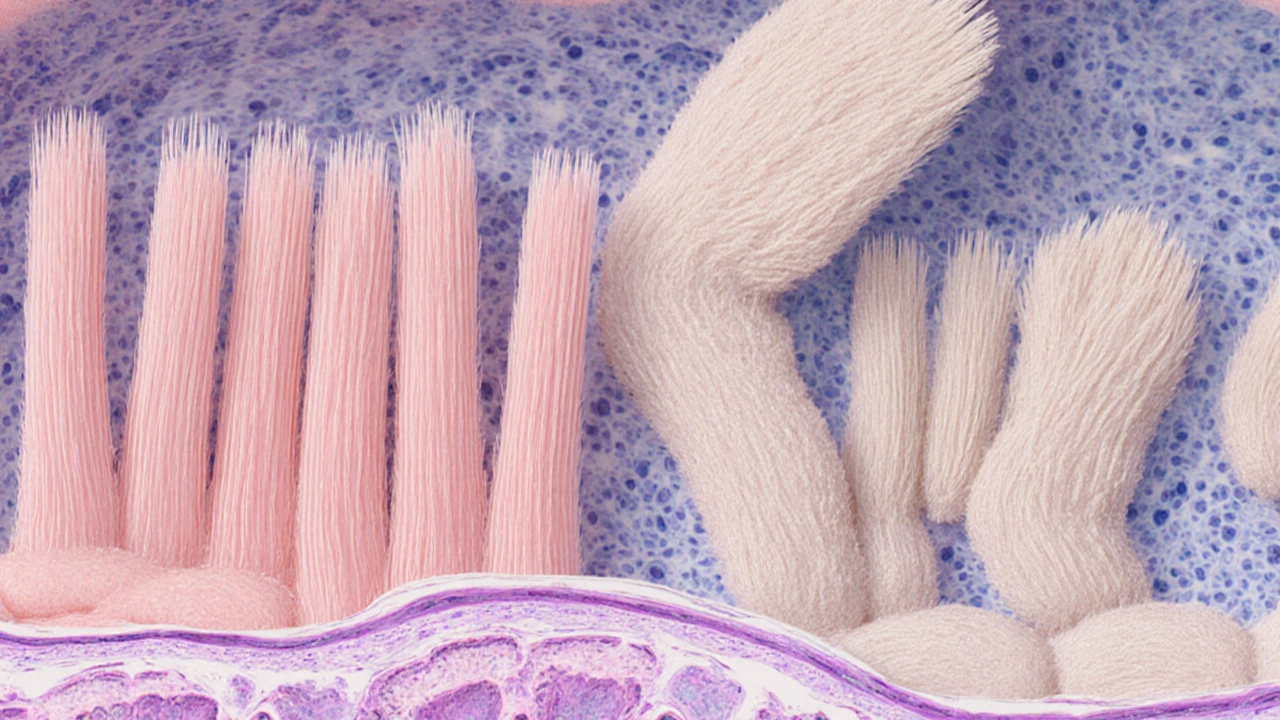
When the lining of the small intestine starts to wear down, digestion trips up, nutrient uptake nosedives, and everyday life can feel like a constant battle with fatigue and bloating. That’s what Atrophic Gastroenteritis is - a condition where the intestinal wall thins and loses its absorptive power. Spotting it early and treating it promptly changes everything from symptom relief to long‑term health outcomes.
TL;DR
- Atrophic gastroenteritis causes malabsorption, weight loss, and vitamin deficiencies.
- Early signs include chronic diarrhea, abdominal pain, and unexplained anemia.
- Endoscopy with biopsy is the gold‑standard for diagnosis.
- Treatment blends dietary changes, nutrient supplements, and, when needed, medication.
- Regular monitoring prevents complications like osteoporosis and neurological issues.
Why Early Diagnosis Matters
Imagine trying to fuel a car with low‑grade gasoline - the engine sputters, performance drops, and damage builds up. Your gut works the same way. If the Small Intestine can’t absorb carbs, proteins, and fats, the body starts pulling from reserves, leading to rapid weight loss and muscle wasting.
Research from the Australian Gastroenterology Society in 2023 showed that patients diagnosed within six months of symptom onset had a 40% lower risk of severe nutrient deficiencies compared with those diagnosed after a year. Early detection also means you can intervene before irreversible villous atrophy sets in.
Key Symptoms You Shouldn't Ignore
- Persistent watery or fatty diarrhea lasting weeks.
- Unexplained iron‑deficiency anemia or low vitamin B12 levels.
- Abdominal cramping after meals, especially with gluten or dairy.
- Unintentional weight loss despite normal calorie intake.
- Neurological tingling or balance problems (often linked to B12 deficiency).
If you tick more than two of these boxes, it’s time to chat with a gastroenterologist. Waiting for the symptoms to “go away” can cost you precious time.
How Doctors Confirm the Diagnosis
The diagnostic pathway combines non‑invasive labs and direct visual assessment. Here’s the step‑by‑step approach most specialists follow:
- Blood tests to check anemia, vitamin D, B12, folate, and inflammatory markers.
- Stool analysis to rule out infections and assess fat malabsorption.
- Endoscopy - a thin camera slides down the throat to the duodenum, allowing doctors to spot mucosal thinning.
- Biopsy of the intestinal lining. Pathologists look for villous atrophy, crypt hyperplasia, and increased intra‑epithelial lymphocytes.
- Optional breath tests for bacterial overgrowth, which can compound malabsorption.
The combination of visual clues and microscopic tissue changes clinches the diagnosis.
Treatment Blueprint: From Food to Pharmacy
Once you know you have atrophic gastroenteritis, the goal is to restore the gut’s absorptive surface and replenish missing nutrients. Treatment typically follows three pillars:
- Dietary adjustments - a gluten‑free, low‑FODMAP plan reduces irritation. Some clinicians also recommend a lactose‑free trial.
- Targeted supplementation - high‑dose vitamin B12 injections, oral iron, calcium, vitamin D, and multivitamins fill the gaps.
- Medication when needed - Proton Pump Inhibitors can lower stomach acidity, giving the damaged lining a chance to heal. In cases linked to autoimmune triggers, low‑dose steroids or immunomodulators may be prescribed.
For patients also dealing with Celiac disease or Crohn's disease, the treatment plan integrates disease‑specific therapies alongside the core atrophy strategy.
Monitoring Progress & Preventing Complications
Even after symptoms improve, the gut needs regular check‑ups. Here’s what a typical follow‑up schedule looks like:
| Time Point | What to Test | Why |
|---|---|---|
| 1 month | Blood levels: B12, iron, calcium | Ensure supplements are effective |
| 3 months | Repeat endoscopy (if severe) | Check mucosal healing |
| 6 months | Bone density scan | Detect early osteoporosis |
| 12 months | Comprehensive metabolic panel | Spot any new deficiencies |
Staying ahead of bone loss, anemia, and neurological decline is the real win. Many patients report feeling “normal” again once labs normalize and weight stabilizes.
Quick Checklist for Patients
- Log daily symptoms - diarrhea frequency, abdominal pain, energy levels.
- Track food intake - note any triggers like gluten, dairy, or high‑fat meals.
- Schedule blood work every 3months during the first year.
- Keep a supplement schedule - dose, type, and timing.
- Attend all follow‑up endoscopies; they’re the best way to see real healing.
Having this list on your phone makes doctor visits smoother and ensures nothing slips through the cracks.

Frequently Asked Questions
Can atrophic gastroenteritis be cured?
While the underlying atrophy may not fully reverse in every case, early treatment can halt progression, restore most nutrient absorption, and dramatically improve quality of life.
Is a gluten‑free diet always required?
Not everyone with atrophic gastroenteritis has celiac disease, but many clinicians start with a gluten‑free trial because gluten can aggravate intestinal inflammation.
How long does it take to feel better after starting treatment?
Most patients notice reduced diarrhea and increased energy within 2-4 weeks, but full nutrient repletion may take 3-6 months.
Are there risks with long‑term supplement use?
High‑dose B12 and iron are generally safe, but excess calcium or vitamin D can cause kidney stones, so monitoring levels is essential.
What lifestyle changes help prevent a relapse?
Maintain a balanced diet, avoid known irritants, stay hydrated, and keep up with regular medical reviews. Stress management and regular exercise also support gut healing.
Bottom line: spotting atrophic gastroenteritis early and kicking off a focused treatment plan can turn a chronic nightmare into a manageable condition. If any of the red‑flag symptoms ring true, act fast - your gut, bones, and brain will thank you.


Early detection of atrophic gastroenteritis can save a lot of hassle and keep you feeling normal. If you notice persistent diarrhea or weird fatigue get checked fast. It’s worth the quick doctor visit.
The article provides a comprehensive overview of the diagnostic pathway, including the necessity of endoscopic biopsy. It correctly emphasizes the importance of timely intervention to prevent irreversible villous atrophy.
Oh great, another reminder that we all love endless endoscopies. Because who doesn’t enjoy swallowing a camera for fun? And those vitamin supplements? Absolutely thrilling. Guess we’ll all be counting our B12 injections like it’s a new hobby.
I concur with the presented management strategy, particularly the integration of dietary modifications alongside supplementation. Collaborative care between gastroenterologists and nutritionists can optimize patient outcomes. A structured follow‑up schedule, as outlined, is essential for monitoring mucosal healing.
Wow, that’s a lot of medical jargon 😒.
Sure, “quick doctor visit” sounds easy until you’re stuck in a waiting room for hours, sipping stale coffee while the nurse asks if you’ve tried a gluten‑free diet for the past decade. The system loves to turn simple red flags into a maze of appointments, and the irony isn’t lost on anyone who’s been through it.
That’s spot on! If you’ve ever wondered how many labs are actually needed, remember that each test brings you closer to nailing the diagnosis. Keep pushing for those answers – the sooner you get clarity, the faster you can start feeling like yourself again.
Really??, you think a camera down your throat is “fun”,??, well‑maybe for some,??, but most of us just want answers, not more stress,!!, and the article could have warned us better,!!
Yeh, the gut is like a little engine of the body, if it sputters everything else slows down. A little bit of mindfulness about food can really boost the healing vibes. Keep the spirit up, the journey to health is a marathon not a sprint.
Don’t you see? The whole “medical guidelines” thing is just a way to keep us in the dark while pharma rolls in cash. People swallow pills without questioning who’s really pulling the strings.
Reading through the detailed breakdown of atrophic gastroenteritis, one cannot help but reflect on how intertwined our daily habits are with the subtle yet profound processes occurring within the small intestine; every bite we take sets off a cascade of enzymatic reactions that, when disrupted, can manifest in ways that are both debilitating and, paradoxically, easily overlooked. The author wisely begins by highlighting the hallmark symptoms-persistent watery diarrhea, unexplained anemia, and that nagging sense of fatigue-that, while common, deserve a heightened level of clinical suspicion when they cluster together. Early diagnosis, as emphasized, hinges upon a multifaceted approach that marries non‑invasive laboratory assessments with the gold‑standard endoscopic biopsy, ensuring that clinicians can visualize and sample the mucosal architecture directly. This dual strategy not only confirms villous atrophy but also helps differentiate atrophic gastroenteritis from other malabsorptive conditions such as celiac disease or Crohn’s disease, a nuance that can dramatically alter therapeutic pathways. The therapeutic blueprint outlined-dietary adjustments, targeted supplementation, and pharmacologic support-mirrors a holistic philosophy that respects the body’s innate capacity for repair when given the proper nutrients and environment. Moreover, the recommendation for a gluten‑free, low‑FODMAP diet, while perhaps daunting to some, underscores the importance of reducing inflammatory triggers early in the treatment timeline. High‑dose vitamin B12 injections, iron therapy, and calcium/vitamin D supplementation are not merely adjuncts but pivotal pillars that safeguard against the cascade of complications that can follow chronic malabsorption, such as osteoporosis, neuropathy, and cognitive decline. The author’s insistence on a structured follow‑up schedule, encompassing periodic blood work, repeat endoscopy, and bone density scans, serves as a reminder that healing is not a linear process but rather a series of checkpoints that inform ongoing management. It is also worth noting that patient education, exemplified by the symptom log and supplement tracker, empowers individuals to become active participants in their own recovery journey. In practice, this collaborative model between gastroenterologists, dietitians, and primary care providers can reduce the time to symptom resolution and improve quality of life metrics substantially. Finally, the article’s concluding call to action-promptly seeking medical evaluation when red‑flag symptoms arise-resonates as a vital public health message, one that could potentially avert years of unnecessary suffering for countless individuals. All in all, the comprehensive nature of this piece not only informs but also inspires a proactive stance toward a condition that is often shrouded in silence.
Honestly, this kind of health advice is universal-our bodies need proper nutrition no matter where we’re from. South Asian diets have long emphasized spices and balanced meals, which can actually help prevent such deficiencies. So the “gluten‑free” hype isn’t the only answer; it’s about respecting traditional food wisdom.
What we’re witnessing here is a textbook case of clinical inertia meeting patient apathy-a perfect storm that drives the pathophysiology of mucosal degeneration into a full‑blown crisis. The interplay of pro‑inflammatory cytokines, epithelial turnover, and micronutrient depletion creates a feedback loop that is, frankly, terrifying.
And let’s not forget the shadowy influence of pharmaceutical conglomerates steering research agendas toward symptomatic treatment rather than true mucosal regeneration. The hidden agenda is palpable when one reads between the lines of sponsored studies.
Another “comprehensive guide” that forgets to mention the cost burden on patients. The diet recommendations sound great until you add up the price of specialty foods and supplements.
Sure thing, the article could’ve thrown in a budget spreadsheet. Some folks can’t afford the “optimal” regimen, so they end up stuck in the same health limbo.
From a philosophical standpoint, the gut is the body’s “second brain,” and ignoring its cries is akin to denying a fundamental aspect of our existential experience. Knowledge of this should compel us to prioritize gut health above superficial concerns.
Indeed, the interrelation between enteric nervous system signaling and systemic homeostasis warrants a multidisciplinary approach. By integrating gastroenterology with neurology, we can better elucidate the bidirectional communication pathways that influence both mental and physical health.
In continuation of the preceding discourse, it is imperative to underscore that regular monitoring, inclusive of periodic endoscopic assessments, hematologic evaluations, and densitometric analyses, constitutes an indispensable facet of comprehensive patient management. ;
Absolutely, maintaining a strict schedule for labs and imaging not only tracks disease progression but also guides therapeutic adjustments, thereby optimizing patient outcomes.