Bladder Emptying: Understanding Causes, Risks, and Solutions
When your bladder emptying, the process of fully releasing urine from the bladder. Also known as voiding, it’s a simple function—until it doesn’t work right. If you feel like you’re never really done, or you have to push, strain, or go again minutes later, you’re not alone. Millions deal with incomplete bladder emptying, and most don’t realize how serious it can get.
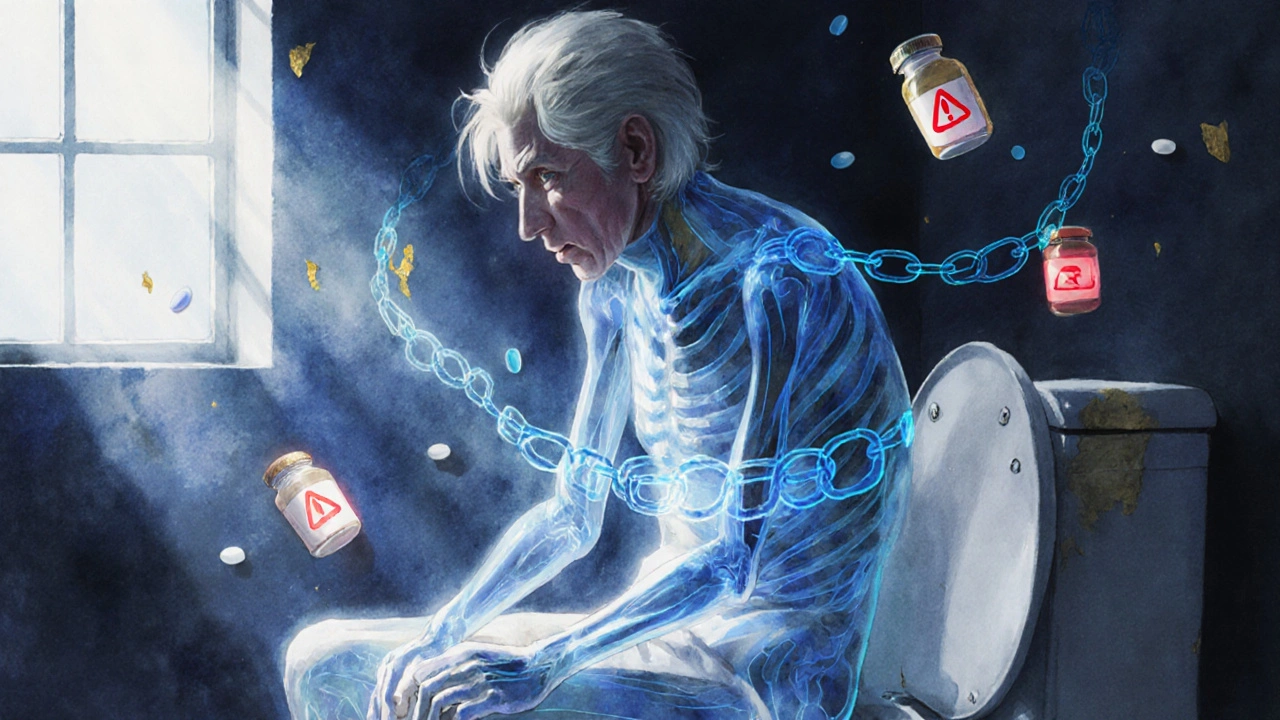
It’s not just about discomfort. When urine stays in the bladder too long, it becomes a breeding ground for urinary tract infections, bacterial infections that start in the bladder and can spread to the kidneys. Left unchecked, this leads to kidney damage, sepsis, or chronic pain. The problem often starts with something small—a nerve issue, a swollen prostate, or weak pelvic muscles. Neurogenic bladder, a condition where nerve signals between the brain and bladder are disrupted. happens after strokes, spinal injuries, or even long-term diabetes. Pelvic floor dysfunction, when muscles that control urination become too tight or too weak. is more common than you think, especially in women after childbirth or men after prostate surgery.
You might think it’s just aging—but that’s not always true. Some people in their 30s have it. Some seniors never do. What matters is whether your bladder is actually emptying, not how old you are. Signs include frequent urination, dribbling after you think you’re done, feeling full even after going, or needing to push or lean forward to finish. If you’re taking medications like antihistamines, antidepressants, or decongestants, they could be making it worse. And if you’ve ever been told your prostate is enlarged, that’s a red flag.
The good news? Most cases can be managed—without surgery. Physical therapy for the pelvic floor, timed voiding schedules, or simple techniques like double voiding (going again after a few minutes) help a lot. Some people need medications to relax the bladder or shrink the prostate. Others need a catheter, temporarily or long-term. But none of that works unless you know what’s really going on. That’s why the posts below cover real cases: how certain drugs affect bladder control, what happens when nerve damage hits, how seniors handle it differently, and what alternatives actually work. You’ll find what works for different causes—not just general advice. This isn’t about guessing. It’s about knowing what’s behind your symptoms, and what to do next.