Psoriasis Causes: Understanding What Triggers This Skin Condition
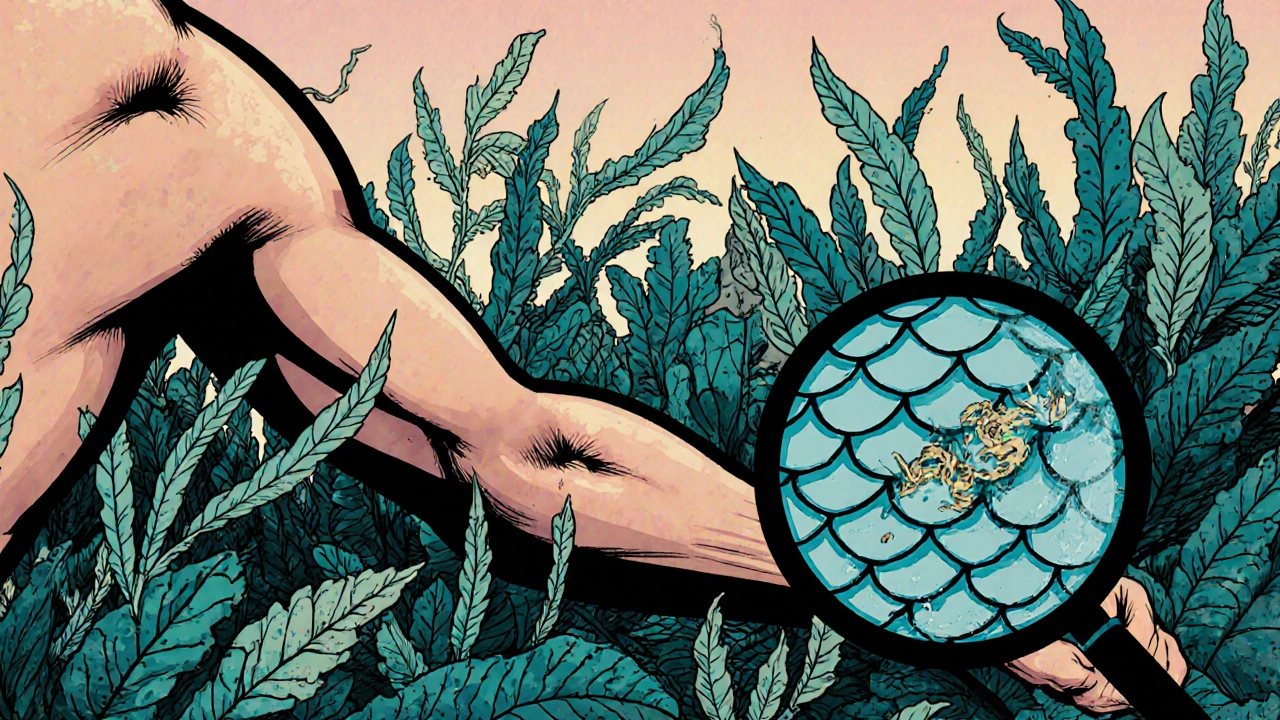
When looking at psoriasis causes, the factors that ignite psoriasis, a chronic inflammatory skin disease affecting millions. Also known as psoriasis triggers, it can appear at any age and often follows a pattern of flare‑ups and remission. The immune system, the body’s defense network that, when overactive, fuels skin inflammation is a central player, while genetics, inherited DNA variations that raise a person’s susceptibility set the stage. Overlaying both is environmental triggers, external factors such as stress, infection, injury or certain medications that can spark a flare‑up. Together, these elements form the core of why psoriasis appears and why it can be stubborn to control.
Think of psoriasis causes as a three‑part puzzle. First, genetics provides the blueprint; studies show that if a close relative has psoriasis, the risk jumps dramatically. Second, the immune system misbehaves, releasing cytokines like TNF‑α and IL‑17 that cause skin cells to grow too fast, creating the classic red, scaly plaques. Third, environmental triggers act like a switch, nudging the immune response over the edge. Stress, for example, can raise cortisol levels, which paradoxically aggravates immune activity in susceptible individuals. Infections such as streptococcal throat infection are notorious for kicking off guttate psoriasis in kids. Even skin injury—a cut or a burn—can lead to a Koebner response, where new lesions form along the wound line. This chain of cause‑and‑effect illustrates the semantic triple: [Psoriasis] requires [immune system dysregulation]; [Genetics] influences [psoriasis susceptibility]; and [Environmental triggers] provoke [psoriasis flare‑ups]. Understanding these links helps you anticipate flare‑ups and choose strategies that target the right point in the chain.
Armed with that knowledge, you can make smarter choices about prevention and treatment. Lifestyle tweaks—like managing stress through mindfulness, keeping a healthy weight, and avoiding smoking—address environmental triggers directly. For those with a strong genetic background, early discussion with a dermatologist about systemic options can keep the immune system in check before plaques spread. Topical therapies, such as prescription steroids or vitamin D analogues, target the inflammation cascade, while newer biologics specifically block cytokines like IL‑17 or IL‑23. Even over‑the‑counter options, like the Flutivate Skin Cream, a potent corticosteroid used for eczema and psoriasis, offer short‑term relief for mild patches. Below you’ll find a curated collection of articles that break down each trigger, dive into the latest research, and share practical steps you can take to keep psoriasis under control.