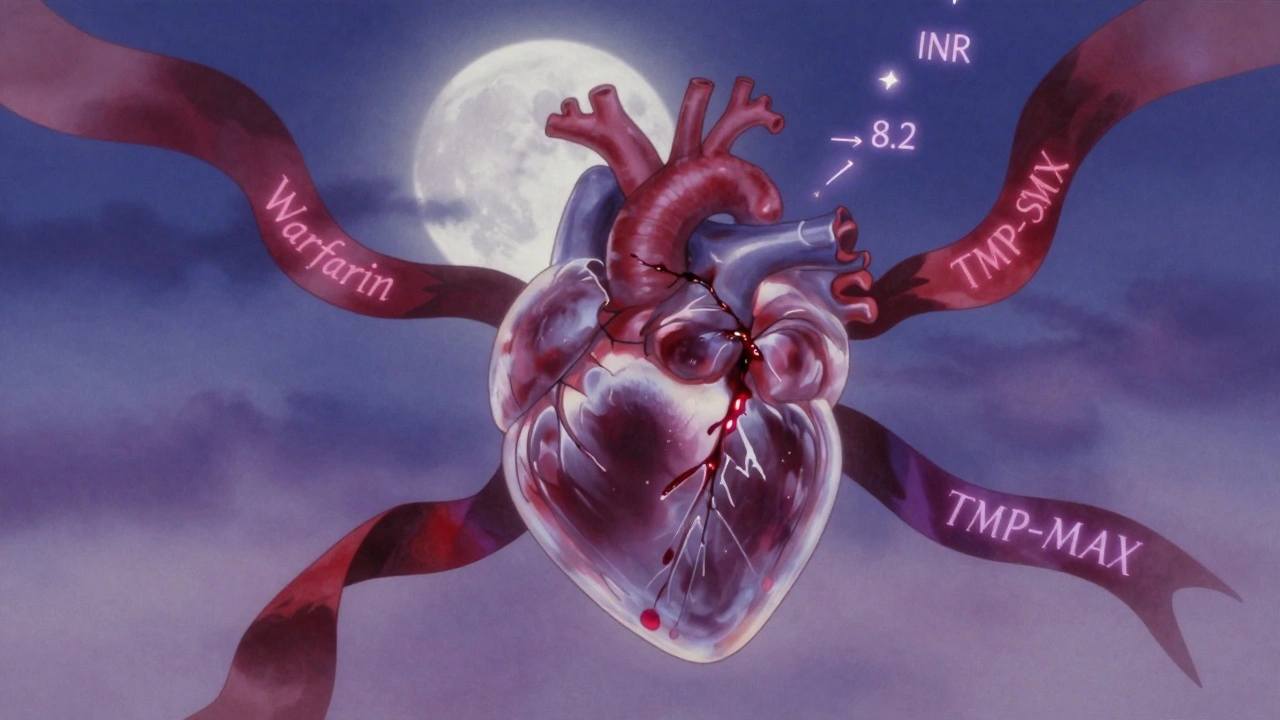
Bactrim and warfarin: Drug interactions you can't afford to ignore
When you take Bactrim, a combination antibiotic made of sulfamethoxazole and trimethoprim, often prescribed for urinary tract infections, sinus infections, or bronchitis along with warfarin, a blood thinner used to prevent clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves, you’re walking a tightrope. This isn’t just a minor caution—it’s a known, dangerous interaction that can lead to serious bleeding, even death. The sulfamethoxazole, the antibiotic component of Bactrim, interferes with how your liver breaks down warfarin, causing warfarin levels to spike. Your INR—a test that measures how long it takes your blood to clot—can jump overnight. One moment you’re fine, the next you’re bruising easily, bleeding from your gums, or passing blood in your stool.
This isn’t rare. Studies show that patients on warfarin who start Bactrim have up to a 50% higher risk of major bleeding within the first week. It’s worse if you’re older, have kidney problems, or already take other meds that affect clotting. Even a short 5-day course of Bactrim can be enough to tip the balance. And here’s the catch: you won’t always feel it coming. No dizziness, no warning. Just a sudden nosebleed, or worse. That’s why doctors often switch you to a different antibiotic—like amoxicillin or doxycycline—if you’re on warfarin. But if you’re already on Bactrim and your doctor doesn’t mention it, ask. Don’t assume it’s safe just because it’s common. Your pharmacist can also flag this combo before you even walk out the door.
If you’re taking both, get your INR checked within 2–3 days of starting Bactrim. Keep a log of any unusual bruising, nosebleeds, dark stools, or headaches. Don’t wait for symptoms. Some people think, "I’ve taken this before," but your body changes. Your diet changes. Your kidneys slow down. That old combo might have been fine last year—but it’s not safe now. The same goes for other antibiotics like ciprofloxacin or metronidazole—they do the same thing. And it’s not just antibiotics. Even some painkillers, supplements like garlic or ginkgo, and over-the-counter cold meds can mess with warfarin. You need a full picture.
Below, you’ll find real stories and data from people who’ve dealt with this exact issue—how they spotted the danger, what their doctors did, and what alternatives actually work. These aren’t theoretical warnings. They’re lived experiences. Whether you’re on warfarin, caring for someone who is, or just trying to avoid a hospital visit, this collection gives you the clear, no-fluff facts you need to stay safe.