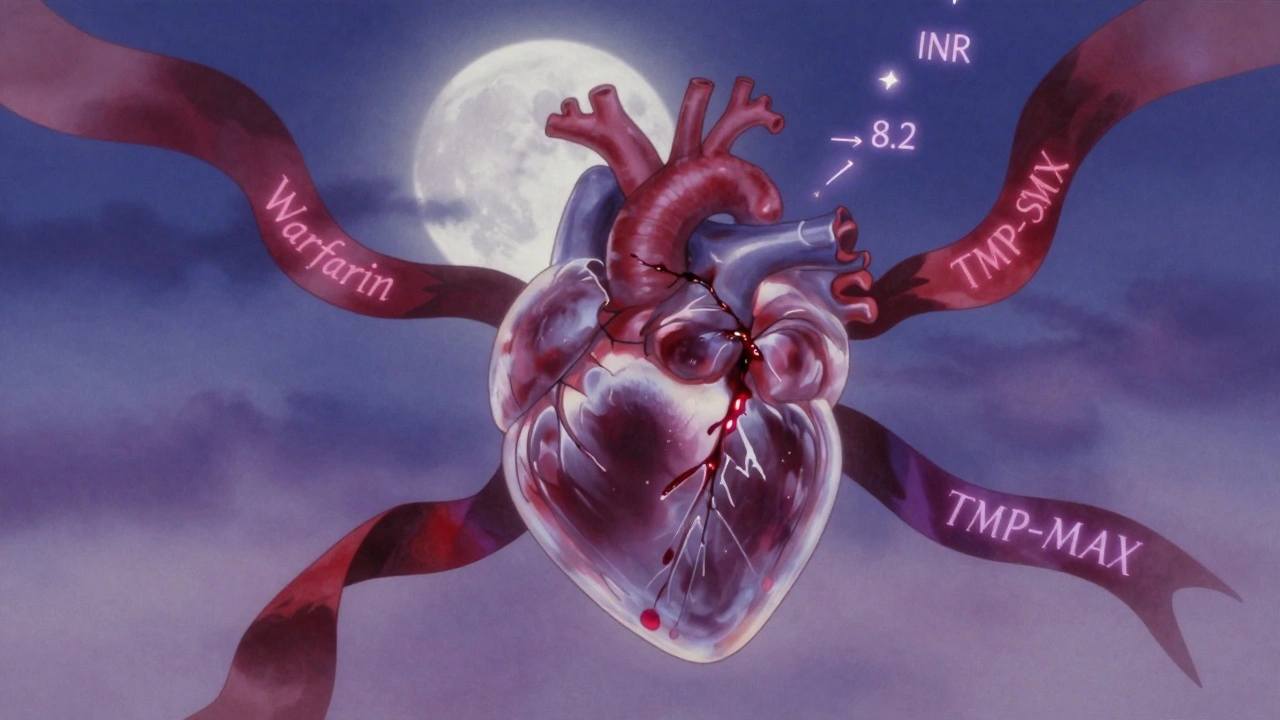
INR Elevation: What It Means, Why It Matters, and How Medications Affect It
When your INR elevation, a measure of how long it takes your blood to clot, that’s higher than normal. Also known as prothrombin time elevation, it means your blood is taking longer than usual to form clots—this can be life-saving if you’re on blood thinners, but deadly if it goes too far. INR stands for International Normalized Ratio, and it’s the standard way doctors track how well anticoagulants like warfarin are working. A normal INR is usually between 2.0 and 3.0 for most people on blood thinners. But when that number climbs above 4.0, you’re at serious risk for uncontrolled bleeding—even from minor injuries.
INR elevation doesn’t happen in a vacuum. It’s often tied to warfarin, a common oral blood thinner used for atrial fibrillation, deep vein thrombosis, and mechanical heart valves. But other drugs can push your INR up unexpectedly. Antibiotics like ciprofloxacin, antifungals like fluconazole, and even some herbal supplements like garlic or ginkgo can interfere with how your body breaks down warfarin. Your liver uses enzymes called CYP2C9 to process it, and anything that blocks those enzymes—whether it’s a prescription, an OTC pill, or a tea—can cause INR to spike. Even something as simple as eating more kale or spinach can lower your INR because vitamin K reverses warfarin’s effect. It’s not about avoiding greens—it’s about keeping them consistent.
People with anticoagulants, medications designed to prevent dangerous clots often don’t realize how many things can throw their INR off. Changes in diet, illness, alcohol use, or even switching from one generic brand to another can cause sudden shifts. That’s why regular blood tests aren’t just routine—they’re critical. An INR of 5.0 or higher might not cause symptoms right away, but it increases your risk of internal bleeding, brain hemorrhages, or fatal bruising. If you’re on warfarin and notice unusual bruising, nosebleeds, dark stools, or headaches, don’t wait—get your INR checked.
The posts below cover exactly these kinds of real-world risks: how common drugs like statins and antifungals interact with blood thinners, what happens when you mix supplements with prescription meds, and how to spot warning signs before an emergency hits. You’ll find practical advice on managing multiple medications, avoiding dangerous combinations, and staying in control even when your body’s chemistry is changing. Whether you’re on warfarin, considering alternatives like DOACs, or just trying to understand why your doctor keeps ordering blood tests, this collection gives you the facts you need—not the fluff.